Authors: Vi Dinh (POCUS 101 Editor), Abigail Beaven, and Rame Bashir.
Patients with Systolic Heart Failure also known as “Heart Failure with Reduced Ejection Fraction (HFrEF)” will commonly present with shortness of breath, orthopnea, paroxysmal nocturnal dyspnea (PND), exercise intolerance, irregular heartbeats, and edema in the bilateral upper and lower extremities. This is usually accompanied by cardiogenic pulmonary edema and B-lines on ultrasound.
One of the most commonly used surrogates in assessing systolic function in these patients is done by measuring the Left Ventricular Ejection Fraction (LVEF).
In this post, we will show you the most common qualitative and quantitative approaches to assess Left Ventricular Ejection Fraction (LVEF) using Point of Care Ultrasound (POCUS) and bedside echocardiography to assess the Systolic Function of your patients.
This is an easy and reliable way to assess left ventricular systolic function in patients ranging from symptoms of chest pain, shortness of breath, myocarditis, to the hypotensive crashing patient.
Table of Contents
Left Ventricular Ejection Fraction (LVEF) Definition
Ejection Fraction (EF) is a percentage of blood pumped by the LV with each contraction. Many factors can affect ejection fraction including preload, afterload, and contractility. A normal EF ranges from 55-69%, and is calculated using the following equation:
Ejection fraction (EF) in percentage is defined as: EF(%) = SV/EDV x 100
Where SV: Stroke Volume and EDV: End Diastolic Volume
Ejection fraction (EF) is basically a percentage, of how much blood the left ventricle pumps out with each contraction. For example, an ejection fraction of 60 percent means that 60 percent of the total amount of blood in the left ventricle is pushed out during each systolic contraction
| Hyperdynamic | Normal | Mildly Reduced | Moderately Reduced | Severely Reduced | |
| Ejection Fraction | >70% | 55-69% | 45-54% | 30-44% | <30% |
Measuring Left Ventricular Ejection Fraction (LVEF) on ultrasound can be approached either qualitatively or quantitatively.
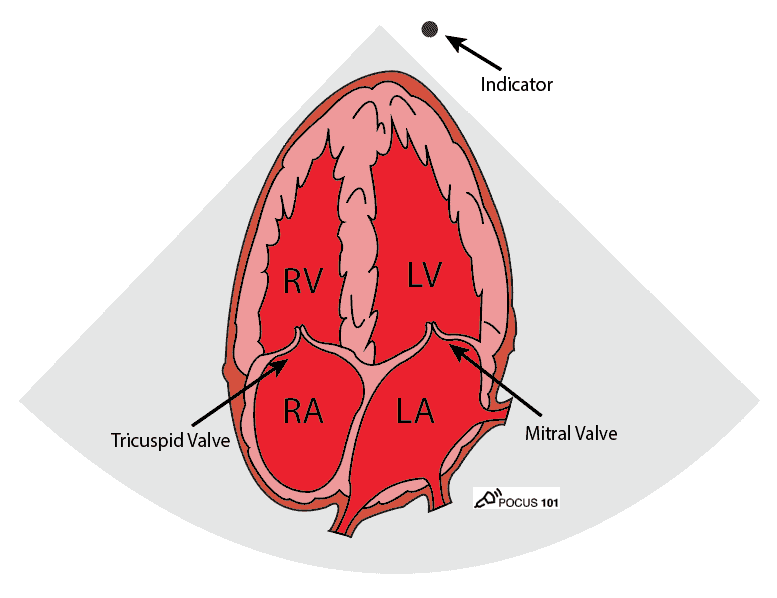
Anatomy and Views
The most common views to assess for left ventricular ejection fraction are the parasternal long axis, parasternal short axis (mid-papillary level), and apical 4 chamber view. The subxiphoid view can also be performed with the parasternal or apical views cannot be obtained. For a complete tutorial on all of the cardiac ultrasound views just click here.
Here is a brief overview of these views.
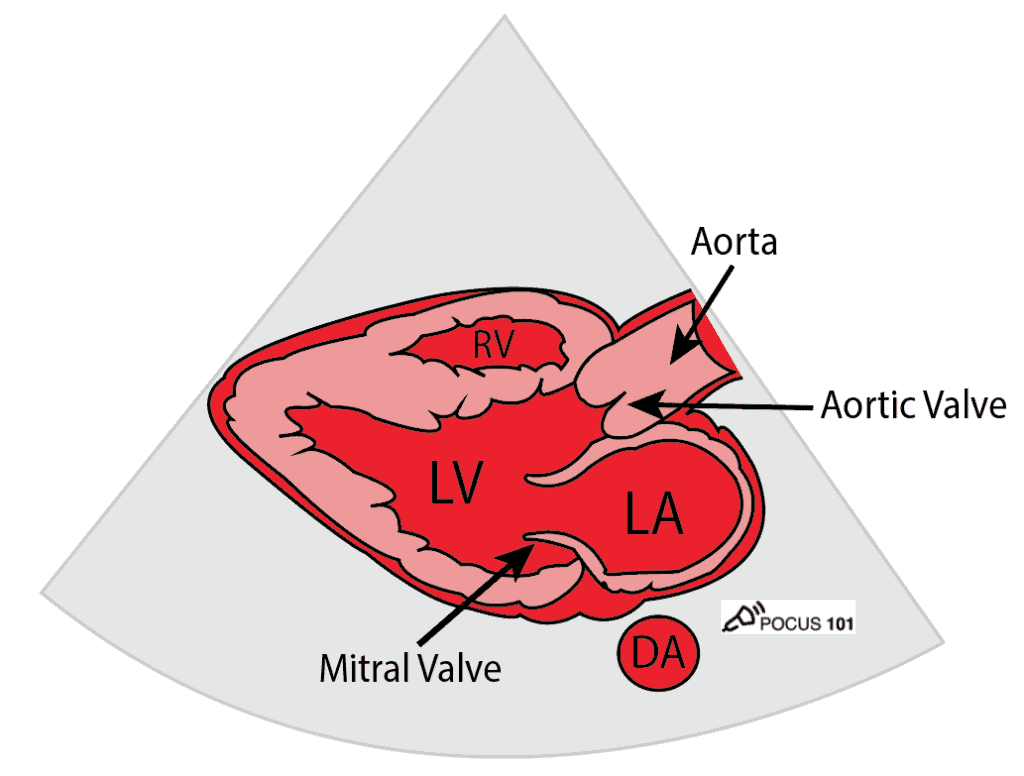
Parasternal Long-Axis (PSLA) View
The heart lays in an oblique orientation, with the left ventricle more posterior than the RV. The Parasternal Long Axis View (PSLA) is used to assess LVEF using fractional shortening and E-point septal separation (EPSS). In this view, the LV is positioned below the right ventricle.
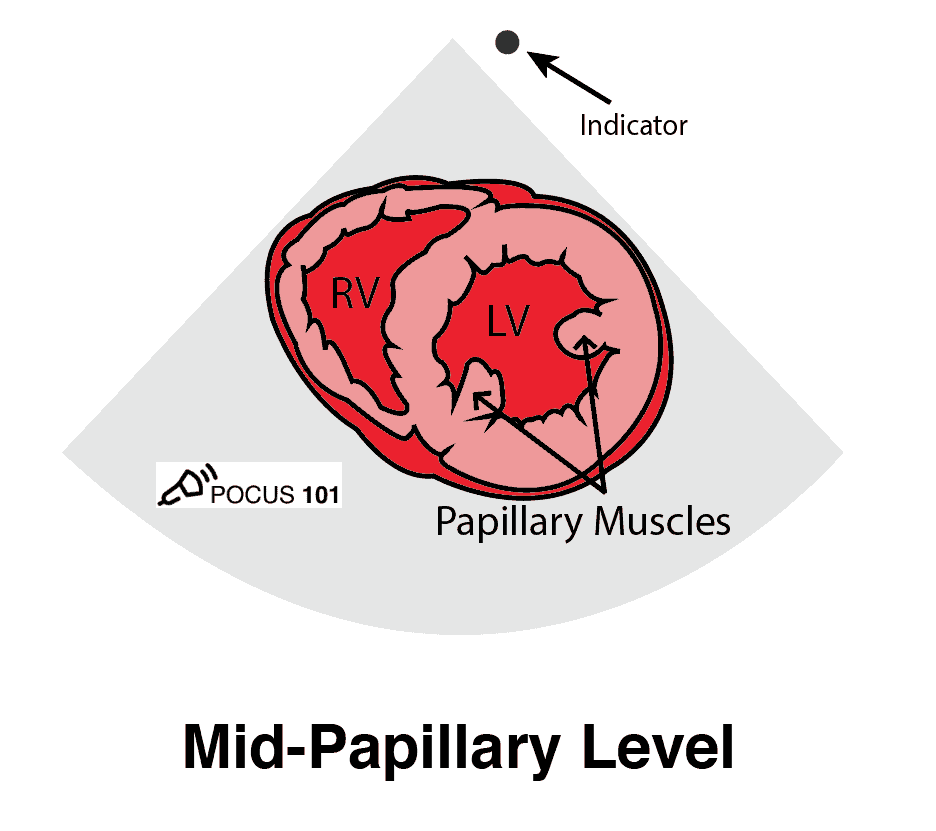
Parasternal Short-Axis (PSSA) View
The parasternal short-axis view (PSSA) gives a cross-section of the heart. To measure fractional area shortening, a PSSA view should be obtained at the level of the papillary muscles.
Apical 4 Chamber (A4C) View
The apical four-chamber view and apical two-chamber view are used in the Simpson’s method to calculate LVEF.
Qualitative Approach to Assessing LVEF
Qualitatively assessing left ventricular ejection fraction allows for rapid assessment of systolic function. Especially when time does not lend itself to time-consuming tracings and calculations. To assess LVEF qualitatively, make observations about both the LV muscle and mitral valve movement.
Surprisingly using qualitative POCUS assessment of ejection fraction correlates with formal echocardiograms fairly well and this is what we normally do in our day-to-day practice.
Here are the two most practical things to assess when looking at LVEF Qualitatively:
- Look at how well the left ventricle walls are moving. Are the LV walls coming close to each other during systole?
- Look at how well the anterior mitral valve leaflet is moving. Is it coming close to the intraventricular septum during diastole?
If the left ventricular walls are moving well and coming close together during systole and the anterior mitral valve leaflet is almost touching the septum during diastole then the patient likely has a normal ejection fraction.
Conversely, if the left ventricular walls are barely moving during systole and the anterior mitral valve leaflet is barely moving during diastole the patient likely has a low ejection fraction.
Qualitative Approach to Assessing Ejection Fraction:
Any cardiac view can be used to look at the qualitatively assess ejection fraction but the two most common are the parasternal long axis and parasternal short axis views.
- Obtain a PSLA view.
- Observe the walls of the left ventricle; are the walls pulling in evenly? Are they pulling in too much, or not enough?
- Observe the mitral valve function; how close does it come to the septum? The closer it comes the better the function.
- Obtain a PSSA view at the mid-papillary level.
- Observe the cardiac muscles in a similar fashion as the PSLA view. Ensure that all sides of the wall are moving inward equally.
- To assist with seeing this, you may place a finger in the center of the ventricle and watch how the wall contracts. This will make hyperdynamic/hypodynamic regions stand out more.
Here are cardiac ultrasound (echo) images of patients with different degrees of ejection fraction from hyperdynamic to severely reduced:
POCUS 101 Tip: The qualitative approach may underestimate true LVEF (Sievers et al., 2005). This technique is operator-dependent but the more you do the more accurate you will become. We would also suggest that when you are first beginning compare your predicted ejection fraction to the formal echo report. Over time you will see you start to correlate pretty well. We’ve found doing this about 10-15 times for a learner should get them a really good idea of estimating LV EF qualitatively.
Quantitative Approaches to Assessing LVEF
There are multiple ways to quantitatively assess for left ventricular ejection fraction. We will go over the most simple ways and then progress to more advanced techniques.
Editors Note: All of these techniques are not absolutely necessary and the majority of the time, even POCUS experts are qualitatively assessing ejection fraction. Quantitative assessment of ejection fraction is not always better as well because if you get the measurement at the wrong angle or cut, it can drastically give you false values. Make sure to understand each technique and its limitations prior to implementing it into your own practice.
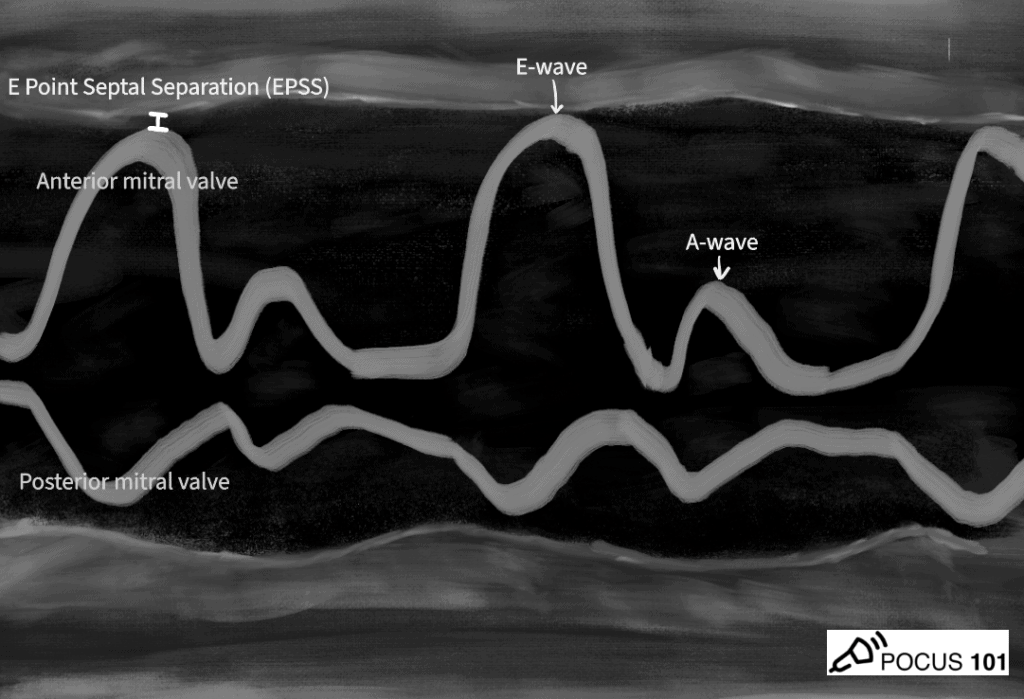
E-Point Septal Separation (EPSS)
E-Point Septal Separation (EPSS) refers to the distance between the anterior leaflet mitral valve and the septum when the mitral valve has reached maximum excursion during early diastolic filling. The larger the EPSS distance the worse the ejection fraction. This correlates to looking at the anterior mitral valve movement with the qualitative assessment.
- The most crucial step in obtaining EPSS is finding a good PSLA view and a horizontally-oriented LV.
- Place the M-mode cursor over the tip of the mitral valve as the anterior leaflet travels towards the LV septum.
- In M-mode, measure the distance between the mitral valve’s “E-wave” (symbolizing the left atrium’s passive filling of the LV) and the LV Septum.
Here is a quick video we made on how to obtain EPSS:
According to cardiac MRI data, EPSS measurements <8mm are considered to have a normal LVEF while distances, 8-18mm are mild/moderately reduced EF, and >18mm are suggestive of severely reduced LVEF (Elagha 2012).
After the EPSS measurement is obtained, it can be also inserted into the following equation to calculate LV ejection fraction (LVEF):
LVEF = 75.5 – (2.5 x EPSS)
Limitations: Obtaining EPSS is limited in pathological diseases that impact the function of the mitral valve (ex: mitral stenosis, mitral valve repair, mitral valve calcification).
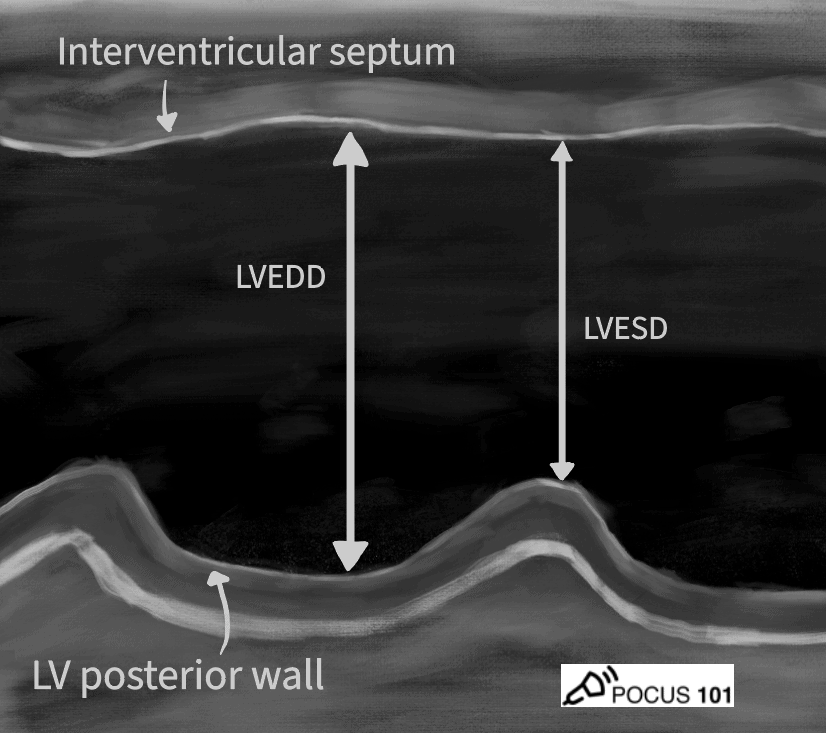
Fractional Shortening
Fractional Shortening is an M-mode measurement of the percent change in diameter between Left Ventricle End Diastole Diameter (LVEDD) and Left Ventricle End Systolic Diameter (LVESD). The following equation allows for the percentage calculation of the size reduction:
FS (%) = (LVEDD-LVESD)/LVEDD x 100
Of note you may also see the machine refer to LVED as LVID or Left Ventricular Inner Diameter.
- Obtain PSLA view
- Select M-mode and place the cursor in the middle of the LV being careful to not include the mitral valve or papillary muscle.
- Freeze the M-mode image.
- Measure the LVEDD (max diameter) and LVESD (minimum diameter)
- The ultrasound will give you an ejection fraction reading.
Here is a video we made with step by step guide on how to do Fractional Shortening.
The caveat is that this value does not express ejection fraction since it is measures a distance and not a volume.
Here is a reference table for fractional shortening:
| Male | Female | |
| Normal EF | 25- 43% | 27- 45% |
| Mildly reduced EF | 20- 24% | 22- 26% |
| Moderately reduced EF | 15- 19% | 17- 21% |
| Severely reduced EF | ≤ 14% | ≤ 16% |
Thankfully you don’t have to remember all of these numbers because the ultrasound machine computes the ejection fraction by converting the diastolic and systolic diameters into volume measurements using the following Teichholz equation:
Vd = [7/(2.4 + LVEDD)] x LVEDD3
Vs = [7/(2.4 + LVESD)] x LVESD3
LVEF = (Vd – Vs)/ Vd
Limitations: For accurate delineation of change in diameter, the M-mode line must cut the LV perpendicularly. This can be ensured with optimal image quality or with the use of an ultrasound machine that enables anatomic M-mode. Other limitations of fractional shortening are evident in certain arrhythmias, in which end-diastole and end-systole are not clearly delineated, making this calculation impossible. Regional wall motion abnormalities also interfere with correct calculation, as the diameter of the left ventricle is not representative of the ventricular size.
Fractional Area Change
Fractional Area Change measures ejection fraction by comparing the area of the left ventricle when viewing the mitral valve function in the Parasternal Short Axis (PSSA) view during systole and at diastole. The normal range is approximately 35-65%.
FAC (%) = (LVEDA-LVESA)/LVEDA x 100
- Obtain PSSAx view at the level of the papillary muscles.
- At the end of diastole (maximum area), measure the area of the left ventricle to obtain the LVEDA.
- At the end of systole (minimum area), measure the area of the left ventricle to obtain the LVESA.
- Insert values into the equation to obtain fractional area change.
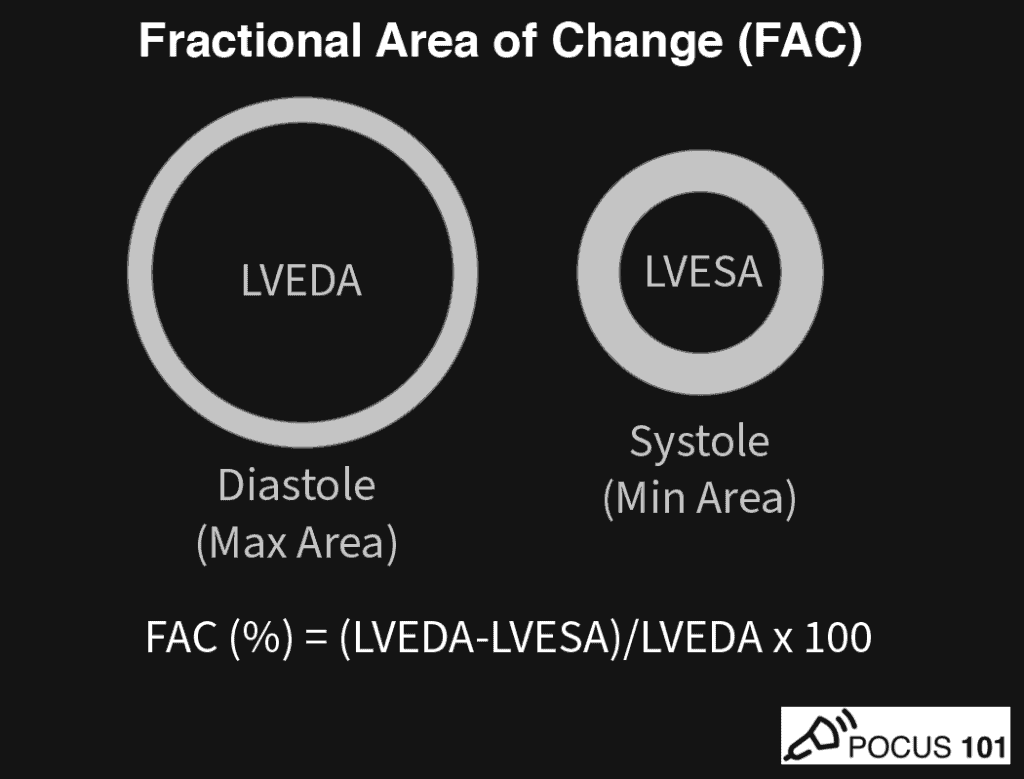
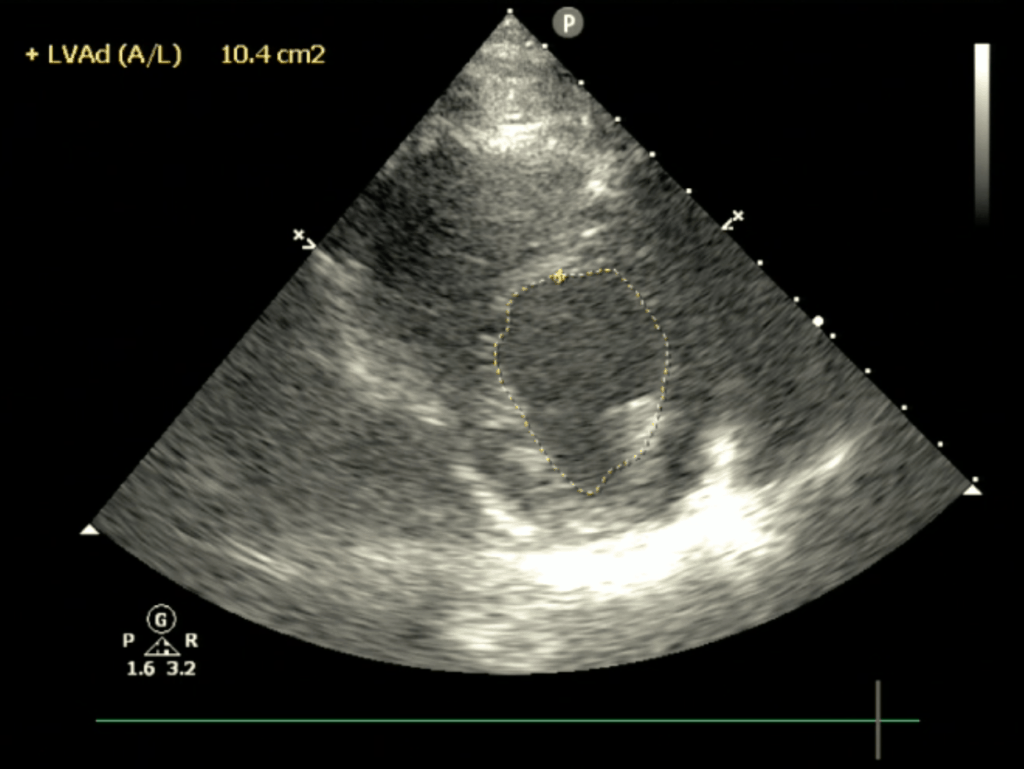
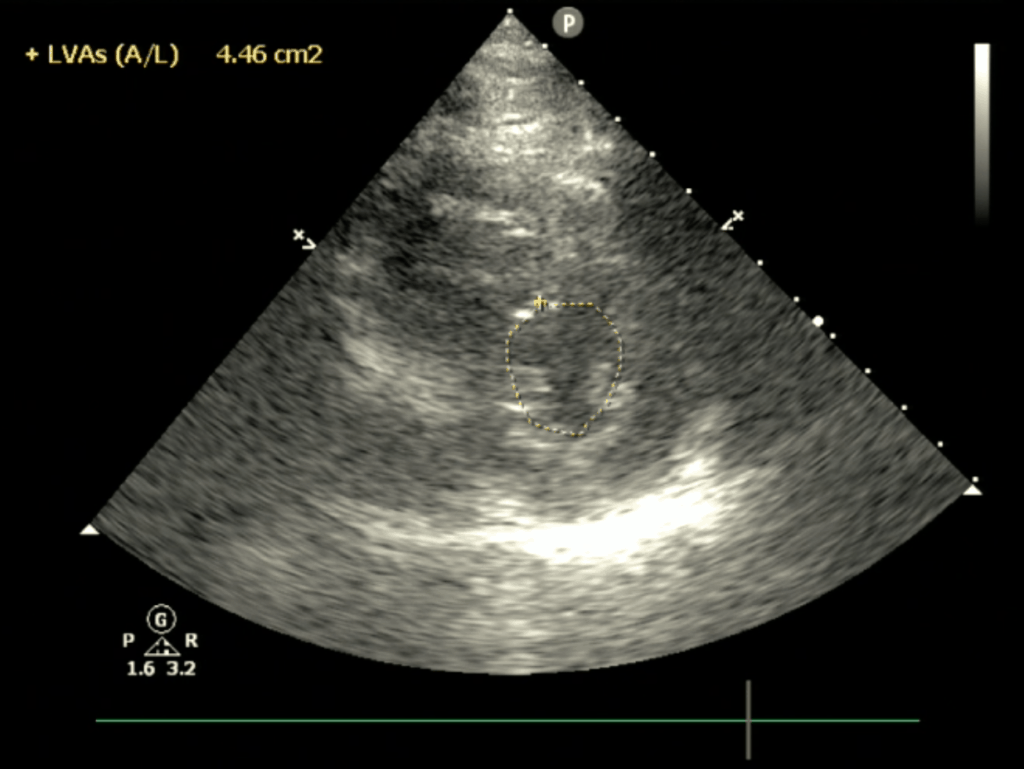
Here is a reference table for how Fractional Area Change correlates to Ejection Fraction:
| Fractional Area Change (FAC) | Ejection Fraction |
| 60% | 75% |
| 50% | 66% |
| 40% | 54% |
| 30% | 42% |
| 20% | 29% |
| 10% | 15% |
Limitations: Regional wall disfunction can alter measurement, and may over- or under-estimate global function.
Simpson (Biplane) Method
The Simpson Method calculates ejection fraction from the entire volume of the left ventricle during systole and diastole (therefore, it is the definition of ejection fraction). It is the best measure of ejection fraction, but it is difficult, time-consuming, and the most operator-dependent technique.
There is no special EF formula for the Simpson Method since it actually measures volumes.
EF = (LVEDV-LVESV)/LVEDV x 100
The reference ranges are:
| Hyperdynamic | Normal | Mildly Reduced | Moderately Reduced | Severely Reduced | |
| Ejection Fraction | >70% | 55-69% | 45-54% | 30-44% | <30% |
The technique involves multiple tracings using the apical 4 and 2 chamber views in both diastole and systole Here is a video that summarizes how to perform the Simpson Method:
Limitations: Although this is the most accurate form of calculating EF, the accuracy of this measurement will depend on image quality. Beware of foreshortening, as this will alter your calculations. Additionally, arrhythmias or regional wall motion abnormalities may not allow for the depiction of end-systole vs end-diastole.
Lastly, one of the greatest difficulties of the Simpson Method is accurately tracing the endocardium correctly and not including other structures such as the papillary muscles. Here is a great video describing how to do this:
References
- Moore CL, Rose GA, Tayal VS, Sullivan DM, Arrowood JA, Kline JA. Determination of left ventricular function by emergency physician echocardiography of hypotensive patients. Acad Emerg Med. 2002 Mar;9(3):186-93. doi: 10.1111/j.1553-2712.2002.tb00242.x. Erratum in: Acad Emerg Med 2002 Jun;9(6):642. PMID: 11874773.
- Sievers B, Kirchberg S, Franken U, Puthenveettil BJ, Bakan A, Trappe HJ. Visual estimation versus quantitative assessment of left ventricular ejection fraction: a comparison by cardiovascular magnetic resonance imaging. Am Heart J. 2005 Oct;150(4):737-42. doi: 10.1016/j.ahj.2004.11.017. PMID: 16209976.
- University of Nebraska Medical Center, Center for Continuing Education. Fractional Area Change. https://e-echocardiography.com/page/page.php?UID=175615601
- Cisewski D, Alerhand S, Singh M. US Prove: E-Point Septal Separation in the CHF patient. emDocs. http://www.emdocs.net/us-probe-e-point-septal-separation-epss-in-the-chf-patient/
- Via G, Hussain A, Wells M, et al. International evidence-based recommendations for focused cardiac ultrasound. J Am Soc Echocardiogram 2014;27(7):683.e1-683.e33.
- Weekes AJ, Tassone HM, Babcock A, et al. Comparison of serial qualitative and quantitative assessments of caval index and left ventricular systolic function during early fluid resuscitation of hypotensive emergency department patients. Acad Emerg Med 2011;18:912-921.
- Elagha, A. & Fuisz, A. Mitral valve E-Point to Septal Separation (EPSS) measurement by cardiac magnetic resonance Imaging as a quantitative surrogate of Left Ventricular Ejection Fraction (LVEF). J Cardiov Magn Reson14, P154 (2012).




Excellent. Easy description.
Thanks a lot.
Absolutely! Thanks for the comment.
Awesome post
Thanks Danielle!!
Concerning the first paragraph, I believe it should be “HFrEF” (not “HFrHF”) , meaning “Heart Failure with reduced Ejection Fraction”
Thanks JJ! I went ahead and made those edits. Appreciate the feedback.
thanks dr…veryx1000 helpfull
i also find it very helpfull with site like ecg weekly by dr amal, and ecg site by dr smith…. is it possible that your team can make a site like that, a case for 1 week with revision and discussion…
Thanks so much! Yes possibly in the future we may create something like that! Thanks so much for the feedback.
Hello,
I was wondering if you would license the Echos for promotional pieces and if so how I would go about it.
Hi Amy. Apologies for the delayed response. What kind of licensing are you looking at? Maybe send me an email at editor@Vi Dinh.com to discuss more. Thanks!
Hi Vi,
Your work and effort here has been amazing. I have pointed my nephrology fellows (and residents/students) to your site several times. You are my goto for pre-reading for hands on session in advanced hemodynamics! Keep up the amazing work.
-Adrian Baudy
Thanks Adrian!! Appreciate the kind words and I’m so happy to hear that this can help with your program! Good luck and thank you for helping to train the next generation of physicians in POCUS!
Is there a typo under EPSS point #3? “In M-mode, measure the distance between the mitral valve’s “E-wave” (symbolizing the left atrium’s active filling of the LV) and the LV Septum.” Should this say “passive” not “active”? Thank you 🙂
WOW. Great catch! I just made the fix. Appreciate it 🙂
Best description I have seen by far!! I’m so excited 😊
Thanks Amanda. Glad it helped!!
Great explanation , easy to understand.
Thanks Pedro!
West or East, You are the best!
Well detailed and easy to comprehend.
Keep that Good Work
Thank you! Appreciate the kind words