Primary Authors: Devin Tooma, Vi Dinh; Co-authors: Jessica Ahn, Jade Deschamps, Satchel Genobaga, Annalise Lang, Victor Lee, Reed Krause, Seth White. Oversight, Review, and Final Edits by Vi Dinh (POCUS 101 Editor).
When encountering a patient with poorly localized abdominal symptoms, the abdomen can seem like a stressful black box with barely a clue to guide your exam.
Point of Care Ultrasound (POCUS) is changing that since it offers you a window into what could be going on. Using POCUS to solve abdominal cases will help you refine your diagnostic skills, streamline your clinical decision making, and confidently check items off your differential – all without even moving your patient to the CT scanner or radiology suite!
In this article, we’ll use an organ-based approach to teach you to perform complete abdomen ultrasound protocol scans of the liver, gallbladder, small and large intestines, appendix, and spleen. We will also explain how to diagnose various abdominal pathologies, and provide a brief overview of some pediatric applications of abdominal ultrasound.
Table of Contents
Indications for Abdominal Ultrasound
Since there are so many organs in the abdominal cavity, it is probably easiest to think of your differential in terms of abdominal quadrants/areas. Below is a list and figure showing some common abdominal diagnoses relative to the abdominal regions.
However, keep in mind that these diagnoses are not confined to just these regions. For example, diverticulitis most commonly presents as left lower quadrant pain, but sometimes can cause pain on the right lower quadrant.
This list and figure are just starting points for you to understand the most common abdominal pathologies and where they usually present.
- Abdominal Pain:
- Right upper quadrant: cholelithiasis, hepatitis, evaluation for free fluid, kidney stones (also flank pain)
- Right lower quadrant: appendicitis, intussusception, psoas abscess, inguinal hernia
- Left upper quadrant: splenomegaly, evaluation for free fluid, kidney stones (also flank pain)
- Left lower quadrant: diverticulitis, small bowel obstruction, inguinal hernia
- Epigastric: AAA, pancreatitis, SBO (can also be generalized)
- Pelvic: urinary retention, pregnancy, ectopic pregnancy, pelvic mass, evaluation for free fluid
- Testicular: torsion, epididymitis, hydrocele.
- Abdominal Trauma: Evaluation for abdominal free fluid (hemoperitoneum)

In this post, we will cover the most common Point of Care Ultrasound (POCUS) applications of abdominal ultrasound including: Hepatobiliary, Spleen, Appendix, Free Fluid Detection, Bowel Emergencies (small bowel obstruction/pneumoperitoneum), and Pediatric specific abdominal applications (pyloric stenosis, intussusception)
We cover Pelvic Ultrasound, Obstetric Ultrasound, Bladder Ultrasound, Renal Ultrasound, and Abdominal Aorta Ultrasound in separate posts (click on the links to go to those posts).
Abdominal Ultrasound Preparation
Patient Preparation
- Your patient should be supine with the head of the bed flat.
- Ask the patient to bend their legs at the knees, if possible, to help relax the abdominal muscles.
- Some applications such as the gallbladder ultrasound exam will require your patient to be on the left lateral decubitus position.
Ultrasound Machine Preparation
- Transducer: Curvilinear Ultrasound Probe (Ideal Choice) or Phased Array Probe.
- You may need to use a Linear Probe for appendicitis and pediatric applications
- Preset: Abdomen
- Machine Placement: Position the ultrasound machine on the right side of the patient with the screen facing you. With this configuration you can face both the patient and the ultrasound screen, scanning with your right hand and manipulating buttons on the machine with the left hand.

Liver Ultrasound
You can use point of care ultrasound of the liver when you encounter a patient with right upper quadrant (RUQ) pain and acute changes in liver function tests.

For the purposes of this abdominal ultrasound guide, the most important measurement to keep in mind is the craniocaudal length of the right lobe. Although liver size varies considerably from patient to patient, depending on age, sex, habitus, and other factors, a healthy liver should be < 16cm in this dimension. This corresponds to roughly the 5th – 11th right intercostal spaces.
Liver Ultrasound Protocol
Using the lateral ultrasound approach, you can assess the size, texture (parenchymal echogenicity), and surface characteristics (capsular contour) of the liver (Rumack). Importantly from this view, the liver also offers a useful acoustic window to view clinically important structures such as the aorta, IVC, hepatic veins, and portal vein.
Position your probe on the patient’s right in the mid-axillary line at the 10th-11th intercostal space, with the indicator facing the patient’s head. If possible, ask your patient to hold their right arm above their head to widen the intercostal spaces.

Visualize the diaphragm, liver, and right kidney in the long-axis.
- Tip: if the ribs are blocking a good view, ask the patient to hold a deep breath to further widen the intercostal spaces. Try rotating your probe obliquely to align with the intercostal spaces as well.

Assess the liver’s echogenicity and capsular contour.
- Normally, the liver has a homogenous echogenicity similar in brightness to the renal cortex (Rumack). Check for notable variations, such as increased or decreased echogenicity, masses, or lesions.
- The liver should have a smooth capsular contour, again similar to that of the kidney. Note any marked coarseness or nodularity.
Measure the liver span in the craniocaudal dimension.
- Once you have visualized the structures listed above, freeze the image and measure the liver span from the diaphragmatic surface to the inferior border, as pictured below.
- POCUS 101 Tip: sometimes, the ultrasound window is too narrow to capture the liver’s diaphragmatic surface and tip together on the screen. Estimate, to the best of your ability, where either of these surfaces would end if you could see them both, and place your calipers at your best guess.

Here is a quick video summarizing how to look for the liver with ultrasound:
Liver Pathology
Scanning the liver using ultrasound has many applications that are beyond the scope of this post. Here, we focus on the findings of acute hepatitis, cirrhosis, and fatty liver disease since they comprise the bulk of liver-related morbidity and mortality (Edlin, Scaglione).
Here is a quick table to help you differentiate between the different liver pathologies on ultrasound.
| Acute hepatitis: | Chronic hepatitis/cirrhosis: | Fatty Liver Disease ( Hepatic Steatosis) |
| ↑ Brightness of portal vein walls ↓ The echogenicity of the liver Usually Enlarged Liver | ↓ Brightness of portal vein walls ↑ Liver echogenicity Usually Small/Atrophic Liver | ↓ Brightness of portal vein walls ↑ Liver echogenicity Usually enlarged Liver |
However, the findings described here for hepatitis and cirrhosis are relatively uncommon findings in the general population and have uncertain operator-dependent sensitivities and specificities. Any ultrasound exam of the liver must be accompanied by a thorough history and physical exam, and inconclusive findings must be bolstered by additional diagnostic modalities.
Acute Hepatitis Ultrasound Findings
In the U.S. alone, over 3 million people have viral hepatitis (hepatitis C > hepatitis B), and over half of those people do not know they have the virus. What’s more, millennials currently represent the most commonly affected population, followed closely by baby boomers. (Office of Infectious Disease).
Acute hepatitis occurs when the liver has an inflammatory reaction to an injury, whether traumatic, infectious, drug-induced, or autoimmune (Joshi). This causes the liver to become edematous and enlarged.
Patients with acute hepatitis most frequently present with acute RUQ pain, fever, jaundice, and elevated liver enzymes (AST/ALT).
Hepatomegaly is the most sensitive POCUS finding in acute hepatitis, defined as a craniocaudal length ≥ 16.0 cm in the midclavicular line (Tchelepi). In addition, the liver may appear relatively hypoechoic versus the adjacent kidney, due to inflammatory fluid buildup in acute hepatitis. This causes the parenchyma to resemble a “starry sky” appearance, whereby the portal vein walls appear as hyperechoic “stars” on a background of dark, edematous hepatocytes. However, this finding has low sensitivity and specificity (Heller).

Reference:https://radiopaedia.org/cases/acute-hepatitis-starry-sky-appearance
Cirrhosis Ultrasound Findings
Cirrhosis results from chronic damage to the liver. In the U.S., excessive alcohol consumption and chronic hepatitis C infection are the most common causes (Muzio). Over half a million Americans are estimated to have cirrhosis, although nearly 70% of them report not knowing they had liver disease. (Office of Infectious Disease).
Symptoms can include ascites, hepatosplenomegaly, jaundice, and dermatological findings such as palmar erythema or spider angiomas.
On ultrasound, you may find surface (capsular) nodularity (88% sensitivity, up to 95% specificity). In addition, the liver will be hyperechoic relative to the right kidney. Other, more difficult findings to assess include right lobe atrophy and caudate lobe hypertrophy (Arger). Keep in mind, however, that the liver may be enlarged in the early stages of cirrhosis, and you will not see atrophy until end-stage disease.

Case courtesy of Dr Chris O’Donnell, Radiopaedia.org. From the case rID: 18858
Fatty Liver Disease (Hepatic Steatosis)
Fatty liver disease or Hepatic Steatosis is a common cause of abdominal pain and elevated liver function test enzymes.
Fatty liver disease can be associated with alcohol abuse, diabetes, obesity, hyperlipidemia, medications (amiodarone, methotrexate, chemotherapy), pregnancy, metabolic disorders, etc.
Hepatic Steatosis ultrasound findings include (Khov 2014):
- Increased liver echogenicity (fat appears echogenic on ultrasound).
- May have enlarged liver size.
- The Renal cortex appears relatively hypoechoic when compared to the liver (the kidney cortex and liver are usually isoechoic).

Gallbladder & Common Bile Duct Ultrasound
Ultrasound is the imaging modality of choice for most biliary tree pathologies. However, since the gallbladder is not fixed to the body wall like other GI organs, it can have a variety of positions in the right upper quadrant (RUQ), so getting a good view can be tricky. Here, we provide a way of imaging this somewhat challenging organ.
Ideally, your patient should fast prior to the exam, so the gallbladder will be dilated with anechoic bile. However, you will most likely have to image the gallbladder in an emergent setting, and fasting will not have been possible.
Gallbladder Ultrasound Protocol
Make sure the patient is fasting. Eating food will make the gallbladder contracted and you may not be able to visualize it. Tip: if possible, have your patient assume the left lateral decubitus position as this will bring the gallbladder more into the midline for your to scan.
- Position your probe in the epigastric midline with the indicator facing the patient’s head.
- In the midline, you will likely see the Main Portal vein in the long-axis, proximal to when it curves into the liver.


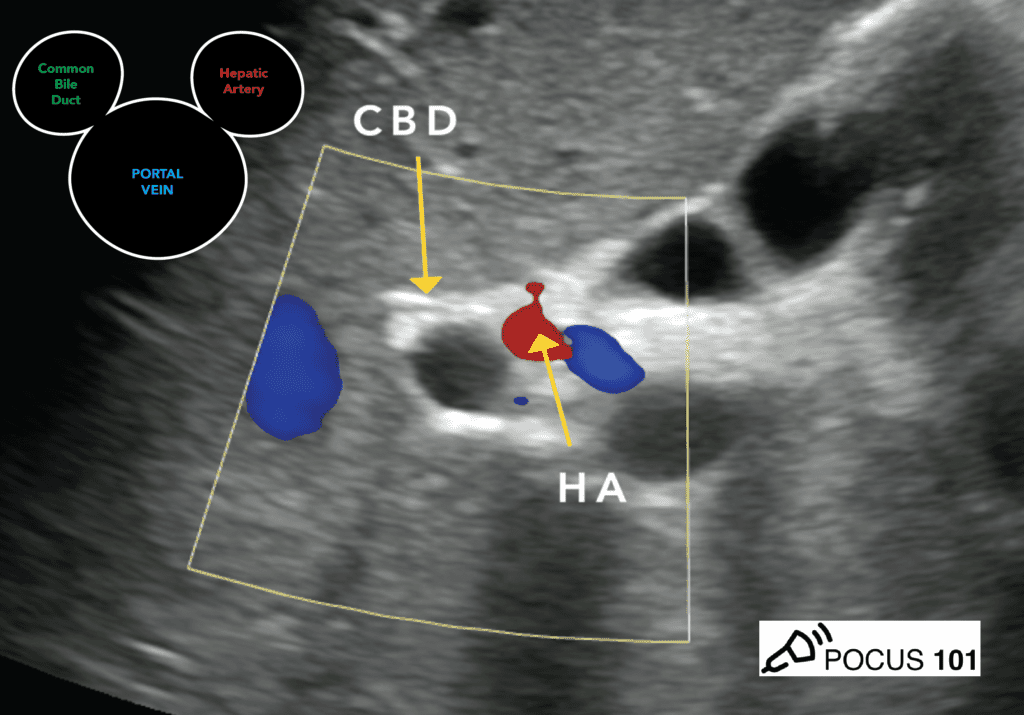
Slide laterally (slowly) along the costal margin, toward the patient’s right, until you can clearly see the Portal Triad (Portal vein, Hepatic Artery, and Common Bile Duct) in short axis.

- The Portal Triad seen in the short-axis is known as the “Mickey Mouse Sign,” where the Common Bile Duct (CBD) and Hepatic Artery are the “ears,” and the portal vein is the “head.”

Visualize the gallbladder and main lobar fissure (MLF).
- The gallbladder neck is attached to the Main Lobar Fissure (MLF). Search adjacent to the MLF, on the right of the screen, by rotating your probe clockwise as shown below.
- This view is known as the “Exclamation Point Sign,” with the portal triad as the “point” and the gallbladder as the “line” of the exclamation.


Evaluate for gallstones.
- Tilt/fan your probe superiorly and inferiorly as shown in the GIF to search for cholelithiasis.

Measure the anterior gallbladder wall thickness.
- Orient your calipers as pictured and measure the anterior gallbladder wall thickness.
- The normal anterior gallbladder wall thickness is <3mm
- Editor’s note: some resources use <5mm thickness to increase the specificity. Remember to use your hospital’s guidelines when measuring.

Evaluate the Common Bile Duct.
- Return to the short-axis view of the portal triad (“Mickey Mouse Sign”) described above.
- Use color Doppler to distinguish the common bile duct from the hepatic artery (proper). Flow will be seen in the hepatic artery, while the common bile duct will remain anechoic with no pulsatile flow.

Visualize the common bile duct in the long axis and measure the anteroposterior diameter.
- From the short-axis view, rotate your probe 90˚ counter-clockwise
- Once you have identified the common bile duct in the long axis, measure it from inner wall to inner wall as shown below.
- A normal CBD measurement is <5mm in the average population
- However, with every decade of life after 50, the expected diameter increases by one millimeter. For example, a 60-year-old patient would be expected to have a CBD around 6mm, and a 70-year-old patient would be expected to have a CBD of 7mm.
- Also, patients that have had their gallbladder removed (cholecystectomy) can have normal CBD measurements of <10mm.


- POCUS 101 Tip: it can be difficult to visualize, let alone measure the CBD. Our quick tip is that if the CBD doesn’t appear wider than 50% the portal vein diameter, it is unlikely any bile duct pathology is present.
Gallbladder/CBD Pathology
Here we’ll cover the most common patient presentations and ultrasound findings for cholelithiasis, cholecystitis, and choledocholithiasis. Ultrasound is by far the preferred initial imaging study for assessing RUQ pain, and boasts high sensitivities and specificities for cholelithiasis and cholecystitis (Revzin).
Cholelithiasis
Cholelithiasis refers to gallstone formation anywhere along the biliary tree. Gallstones are present in up to 10% of the population, and only about 1/4 of patients are symptomatic. When symptomatic, the most common finding is biliary colic (post-prandial RUQ pain, especially following a fat-rich meal). Pain may radiate to tip of the right scapula, a finding known as Collin’s sign. Nausea, bloating, belching, heartburn, and flatulence are also common (Bell).
Ultrasound is considered the gold standard for the detection of gallstones (Kothari), which will appear as highly hyperechoic collections with posterior shadowing within the gallbladder lumen. The stones may be gravity-dependent (“rolling stones”) and move within the lumen when the patient changes position.

Smaller stones may not be directly visible within the lumen, but may exhibit a “twinkling artifact” with color Doppler, pictured below. On the right, the tiny stone is visible in grayscale (green arrow).

Cholecystitis on Ultrasound
Cholecystitis, or gallbladder inflammation, occurs when the gallbladder’s drainage ducts are obstructed and the gallbladder becomes inflamed/infected. Cholelithiasis is the most common cause and primary risk factor for developing cholecystitis, implicated in up to 95% of cases of cholecystitis (Liau). Other causes (acalculous cholecystitis) include sludge (fine bile crystals mixed with proteinaceous debris and fluids) or tumors.
Patients with cholecystitis most commonly present with acute RUQ pain, persistent over ≥ 6 hours, that may radiate to the right shoulder. Nausea, vomiting, and fever are also common. Lab abnormalities can include leukocytosis and increased liver function tests.
The cardinal physical exam finding for cholecystitis is the traditional Murphy’s sign on physical exam. With your fingers clasped under the right costal margin, a positive Murphy sign refers to a “catch” in the patient’s breath when asked to inhale deeply, indicating pain when the gallbladder touches the examiner’s fingers.
A Sonographic Murphy sign, however, refers to the presence of maximal tenderness when ultrasound probe pressure is applied over the visualized gallbladder on ultrasound. This is a very sensitive finding for cholecystitis (Bree).

Important secondary findings include cholelithiasis (gallstones), anterior gallbladder wall thickening >3mm, and pericholecystic fluid.
Other less specific findings are gallbladder sludge and gallbladder distension (>4cm transverse and >9cm longitudinal).

Case courtesy of Dr Maulik S Patel, Radiopaedia.org. From the case rID: 20542
Choledocholithiasis
Choledocholithiasis occurs when gallstones lodge in the bile ducts and bile can no longer flow, instead backing up into the liver. Most cases are symptomatic and require removal of the stones since ascending cholangitis (acute bacterial infection of the biliary tree) is a common complication with high morbidity/mortality.
Patients with choledocolithiasis usually present with biliary colic and obstructive jaundice, ascending cholangitis, and potentially acute pancreatitis (Hartung).
On ultrasound, look out for calculi in the gallbladder and/or CBD, and a dilated common bile duct. Any CBD wider than 5mm should raise suspicion, especially when paired with a suggestive history. However, with every decade of life past 50, the expected diameter increases by one millimeter. For example, a 60-year-old patient would be expected to have a CBD around 6mm, and a 70-year-old patient would be expected to have a CBD of 7mm.

Case courtesy of Dr David Cuete, Radiopaedia.org. From the case rID: 43915
Spleen Ultrasound
The spleen is imaged from the patient’s right side using ultrasonography. As with the liver, the spleen can be used as an acoustic window to assess other important structures, such as the aorta and IVC. Here, you’ll learn how to visualize the spleen and measure its craniocaudal length to evaluate for splenomegaly.
Spleen Ultrasound Protocol
- Place your probe in the 7th-8th intercostal space on the patient’s left side, with the indicator facing the patient’s head.
- The spleen lies quite posteriorly, so you’ll want to be “knuckles-to-bed” to properly visualize it.

Visualize the spleen and adjacent left kidney.
- If the ribs are casting a shadow over your window, try having the patient hold a deep breath to further widen the intercostal spaces. Align your probe obliquely with the intercostal space by rotating slightly clockwise.
Measure the spleen in the craniocaudal dimension. This is to evaluate for splenomegaly.
- If you cannot see the superior and inferior boundaries of the spleen, estimate as shown below.
- A normal spleen measurement is <12-14cm.


Here is a short video going over how to evaluate the spleen using abdominal ultrasound:
Splenomegaly
There are numerous etiologies of splenomegaly, which can be broadly categorized as hematological (anemias, hematological neoplasms), hemodynamic (such as portal vein obstruction), infectious (especially viral), metabolic, neoplastic (non-hematological metastases), and owing to connective tissue disorders.
Since the etiologies are so varied, the associated manifestations will also vary widely from patient to patient. In rare cases, you may be able to appreciate a palpably enlarged spleen on physical exam. Patients may also complain vaguely of dull LUQ pain, fatigue (from anemia), and abdominal fullness.
A healthy spleen has a homogeneous echogenicity, smooth capsular contours, and a craniocaudal length no more than 12cm in an adult (although taller males may have a spleen up to 14cm long). Any larger, and your patient likely has splenomegaly.
Other findings in splenomegaly include a rounded inferior splenic surface – note above how the spleen sort of “hugs” the kidney and is convex inferiorly, whereas in the image below, the bottom has become concave with respect to the kidney, also dwarfing it in size.

Case courtesy of Dr Ian Bickle, Radiopaedia.org. From the case rID: 52825
Appendix Ultrasound
As one of the most common conditions prompting an ED visit, appendicitis is a pathology you are certain to encounter. And it’s a pathology you certainly don’t want to miss, given the complications associated with perforation.
Indications for performing an ultraosund exam of the appendix include the following common signs and symptoms:
- Focal RLQ pain
- Rebound tenderness/signs of peritoneal irritation
- Pelvic pain
- Fever
- Elevated WBC count
The appendix is located in the right lower quadrant, attached to the cecum. However, its location can vary widely in its anatomic position, as pictured below.

Appendicitis Ultrasound Protocol
Acute appendicitis is the most common abdominal emergency, representing 250,000 cases annually, and a lifetime prevalence among men and women of 9% and 7%, respectively (Mostbeck).
However, diagnosing appendicitis is a challenge, despite its prevalence. Symptoms are often non-specific, overlapping with various abdominal pathologies. And finding the appendix can be tricky, especially since the appendix can be located retrocecally.
This makes ultrasound less sensitive (~84%) for detecting appendicitis – failing to identify the appendix does not exclude it. However, POCUS is highly specific for appendicitis (~96%), and it should be your first-line imaging modality when you suspect it (Al-Khayal).
The most common presenting symptom of appendicitis is abdominal pain. The pain starts as dull periumbilical pain, then localized about a day later as sharp, stabbing pain at McBurney’s point, or 1/3 the distance of a line drawn between the anterior superior iliac spine and the umbilicus.

There are two ways to go about the appendix POCUS exam, described below. We recommend starting with the “point of maximal tenderness” method, then using a more systematic approach to finding the appendix if the first method isn’t successful.
First, position your patient and select your probe.
- Probe selection: linear probe for a child/thin adult, or curvilinear probe for any patient with a large BMI.
- Preset: Superficial/Abdomen
Option 1: Point of Maximal Tenderness
This is our preferred method when you strongly suspect appendicitis based on your patient’s history and physical exam.
Have your patient point, as precisely as possible, to “where it hurts” – the point of maximal tenderness.
- Place the probe on the point of maximal tenderness with the indicator towards the patient’s right.
- Attempt to locate the appendix as a non-compressible structure with a blind-ended pouch.
- Rotate the probe to attempt to find the appendix in long and short-axis views.
- Look for the signs of Appendicitis on Ultrasound described below.
Option 2: Systematic Approach
If you prefer a more organized approach, try starting in the RUQ, again with the probe in the transverse orientation with the indicator facing the patient’s right.
- Trace the ascending colon downward until reaching the cecum, and have identified the psoas major and the iliac vessels, as seen below.
- Now, search slightly medial to the psoas muscle for the ultrasound findings of appendicitis described below.


POCUS101 Tip: if bowel gas is obscuring the image, use graded compression, and watch the patient’s eyes for any signs of discomfort as you apply pressure. The appendix can be especially difficult to visualize in patients with a large habitus. Keep in mind that the appendixes can be retrocecal, thus will be obscured from view when there is gas in the ascending colon.
Appendicitis Ultrasound Findings:
- Non-compressibility of the appendix (unless perforated)
- Blind ended pouch
- Diameter of the appendix > 6 mm
- Single wall thickness ≥ 3 mm
- Target sign
- Hyperechoic appendicolith with posterior shadowing



Abdominal Free Fluid Ultrasound
Evaluating for free fluid is a common abdominal ultrasound application. We will go over the most common locations to detect free fluid using abdominal ultrasound.
Using these techniques, you’ll be able to diagnose ascites and hemoperitoneum in trauma patients (read the complete eFAST exam tutorial HERE). Keep in mind that blood will look more echogenic as hemoperitoneum progresses and begins to coagulate.
Right Upper Quadrant (RUQ) – Morison’s Pouch
- Using the technique to scan the liver described above, you can detect free abdominal fluid in the hepatorenal recess (Morison’s Pouch). Normally, the recess is only a potential space, and no anechoic fluid should be seen between the liver and kidney.


Left Upper Quadrant – Perisplenic Recess
- Using the technique to scan the spleen described above, you can detect free abdominal fluid in the perisplenic recess. You can also check the costodiaphragmatic recess from this view.


Male Pelvis – Retrovesical Pouch
In the male pelvis, you can find free fluid in the rectovesical pouch/space.


Female Pelvis – Pouch of Douglas
In the female pelvis, you can find free fluid in the Pouch of Douglas (Rectouterine Pouch).


Small Bowel Obstruction Ultrasound
Small Bowel Obstruction (SBO) is a common type of mechanical GI obstruction, representing 80% of cases (versus 20% large bowel obstruction). Ultrasound can be used to detect SBO (Taylor).
Classic signs and symptoms for SBO include cramping abdominal pain, and abdominal distension with nausea.
The ultrasound technique for detecting SBO is known as “mowing the lawn” or the “lawnmower technique”. Starting in the RLQ and using graded compression, slowly scan the abdominal quadrants as depicted below.

Ultrasound findings for small bowel obstruction include:
- Dilated bowel loops (diameter > 3cm)
- Ineffective or absent peristalsis, which will be seen as a “whirling” of intra-luminal contents
- Collapsed colonic lumen
When 2 of 3 of these findings are present, POCUS has sensitivities and specificities of over 90% to detect SBO (Unlüer et al).

(Unlüer et al)
Pneumoperitoneum Ultrasound
Pneumoperitoneum is free air within the peritoneal cavity. It has various etiologies and is easily confused with several other causes of acute abdominal pain. Etiologies can broadly be classified as traumatic or non-traumatic. Traumatic causes of pneumoperitoneum include iatrogenic injuries or stab wounds. Non-traumatic causes are numerous, including perforated ulcer, infection, erosion, and ischemia.
The most common cause of pneumoperitoneum is the perforation of a hollow viscus, such as in a perforated stomach ulcer (Tanner).
On abdominal ultrasound, the most common finding for pneumoperitoneum is the Enhanced Peritoneal Stripe Sign (EPSS). This is when air within the peritoneal space rises and causes an “echoing” of the usually single, hyperechoic peritoneal stripe that separates the abdominal wall from underlying peritoneal fluid and fluid-filled organs (Indiran).
If there is a large amount of pneumoperitoneum, your image of abdominal organs will be obscured by gas wherever you place your probe.

Pediatric Abdominal Ultrasound Applications
Abdominal ultrasound has numerous pediatric applications. Here, we focus on appendicitis vs mesenteric adenitis, pyloric stenosis, and intussusception.
Appendicitis vs Mesenteric Adenitis
Our technique for detecting appendicitis is described in the section above.
An important differential diagnosis in appendicitis includes mesenteric adenitis. In contrast to appendicitis, ultrasound findings for mesenteric adenitis will be the absence of a visibly enlarged appendix, and the presence of enlarged mesenteric nodes, as pictured below.

Case courtesy of Dr Chris O’Donnell, Radiopaedia.org. From the case rID: 18049
Pyloric Stenosis Ultrasound
Pyloric stenosis refers to idiopathic, hypertrophic thickening of the pyloric musculature, which progresses to gastric outlet obstruction. Symptoms typically present at 2-8 weeks of age. Classically, this will feature a neonate with non-bilious, projectile vomiting. You may also appreciate an olive-sized mass in the right upper quadrant on physical exam.
On ultrasound, the diagnosis of pyloric stenosis is based on 2 measurements: a pyloric muscle diameter > 4mm, and a pyloric canal length > 14mm.


Intussusception Ultrasound
Intussusception occurs when a segment of bowel “telescopes” onto another segment, or onto itself, because of peristalsis. It is a common cause of acute abdomen in children, the most common cause of intestinal obstruction in children, and has significant complications, such as bowel necrosis, making its timely detection imperative (Edwards).
The classic triad of intussusception is intermittent abdominal pain, vomiting, and the presence of a right upper quadrant mass. When paired with the presence of gross or occult bleeding on rectal exam, this has a high positive predictive value for intussusception.
POCUS has high sensitivity and specificity for detection of intussusception (97.9% and 97.8%, respectively), as well as a high negative predictive value (99.7%; Edwards).
The most common ultrasound findings for intussusception are:
- Target sign: inflamed bands of hyperechoic mucosa and relatively hypoechoic submucosa are visible.
- Pseudokidney sign: fat-containing mesentery is dragged into the intussusception, resembling the kidney hilum. The resultant longitudinal appearance is of a small kidney.

Case courtesy of Dr Behrang Amini , Radiopaedia.org. From the case rID: 3456

Case courtesy of Dr T Menezes, Radiopaedia.org. From the case rID: 33056
References
- Noble, V. E., & Nelson, B. (2014). Manual of Emergency and Critical Care Ultrasound. Cambridge, UK, MA: Cambridge University Press.
- Rumack, Carol M., and Levine, Deborah. Diagnostic Ultrasound E-Book. United Kingdom, Elsevier Health Sciences, 2017.
- Arger, Peter, & Benson, Carol. Ultrasound, a practical approach to clinical problems. Thieme Publishing Group. (2008) ISBN:3131168323.
- Edlin BR, Eckhardt BJ, Shu MA, Holmberg SD, Swan T. Toward a more accurate estimate of the prevalence of hepatitis C in the United States. Hepatology. 2015 Nov;62(5):1353-63. doi: 10.1002/hep.27978. Epub 2015 Aug 25. PMID: 26171595; PMCID: PMC4751870.
- Office of Infectious Disease and HIV\/AIDS Policy (OIDP). (2016, June 7). Viral Hepatitis in the United States: Data and Trends. HHS.Gov. https://www.hhs.gov/hepatitis/learn-about-viral-hepatitis/data-and-trends/index.html
- Scaglione S, Kliethermes S, Cao G, Shoham D, Durazo R, Luke A, Volk ML. The Epidemiology of Cirrhosis in the United States: A Population-based Study. J Clin Gastroenterol. 2015 Sep;49(8):690-6. doi: 10.1097/MCG.0000000000000208. PMID: 25291348.
- Macnaught F, Campbell-Rogers N. The liver: how we do it. Australas J Ultrasound Med. 2009;12(3):44-47. doi:10.1002/j.2205-0140.2009.tb00061.x
- Normal Liver Ultrasound How To. (2020). Retrieved August 12, 2020, from https://www.ultrasoundpaedia.com
- Heller MT, Tublin ME. The role of ultrasonography in the evaluation of diffuse liver disease. Radiol Clin North Am. 2014;52(6):1163-1175. doi:10.1016/j.rcl.2014.07.013
- Tchelepi H, Ralls PW, Radin R, Grant E. Sonography of diffuse liver disease. J Ultrasound Med. 2002;21(9):1023-1034. doi:10.7863/jum.2002.21.9.1023
- Lurie, Yoav et al. Non-invasive diagnosis of liver fibrosis and cirrhosis. World journal of gastroenterology vol. 21,41 (2015): 11567-83. doi:10.3748/wjg.v21.i41.11567
- Khov, N., Sharma, A., Riley, T. (2014). Bedside ultrasound in the diagnosis of nonalcoholic fatty liver disease World Journal of Gastroenterology 20(22), 6821-6825.
- Case courtesy of Dr Bruno Di Muzio, Radiopaedia.org. From the case rID: 80805
- Joshi, G., Crawford, K., Hanna, T., Herr, K., Dahiya, N., Menias, C. (2018). US of Right Upper Quadrant Pain in the Emergency Department: Diagnosing beyond Gallbladder and Biliary Disease RadioGraphics 38(3), 766-793.
- Pinto, A., Reginelli, A., Cagini, L. et al. Accuracy of ultrasonography in the diagnosis of acute calculous cholecystitis: review of the literature. Crit Ultrasound J 5, S11 (2013). https://0-doi-org.catalog.llu.edu/10.1186/2036-7902-5-S1-S11
- Revzin, M., Scoutt, L., Garner, J., Moore, C. (2017). Right Upper Quadrant Pain: Ultrasound First! Journal of Ultrasound in Medicine 36(10), 1975-1985 https://dx.doi.org/10.1002/jum.14274
- Liau, K., Teh, C., & Serrablo, A. (2014). Management of acute cholecystitis and acute cholangitis in emergency setting, Open Medicine, 9(3), 357-369. doi: https://doi.org/10.2478/s11536-013-0301-3
- Bree, RL. Further observations on the usefulness of the sonographic Murphy sign in the evaluation of suspected acute cholecystitis. J Clin Ultrasound. 1995 Mar-Apr;23(3):169-72. doi: 10.1002/jcu.1870230304. PMID: 7730462.
- Bell, D., & Sorrentino, S. (2012). Gallstones: Radiology Reference Article. Retrieved October 05, 2020
- Kothari, S. N., Obinwanne, K. M., Baker, M. T., Mathiason, M. A., & Kallies, K. J. (2013). A Prospective, Blinded Comparison of Laparoscopic Ultrasound with Transabdominal Ultrasound for the Detection of Gallbladder Pathology in Morbidly Obese Patients. Journal of the American College of Surgeons, 216(6), 1057-1062. doi:10.1016/j.jamcollsurg.2013.02.009
- Hartung, M., & Gaillard, F. (2010). Choledocholithiasis: Radiology Reference Article. Retrieved October 05, 2020
- Mostbeck, G., Adam, E. J., Nielsen, M. B., Claudon, M., Clevert, D., Nicolau, C., Nyhsen, C., & Owens, C. M. (2016). How to diagnose acute appendicitis: ultrasound first. Insights into imaging, 7(2), 255–263. https://doi.org/10.1007/s13244-016-0469-6
- Al-Khayal KA, Al-Omran MA. Computed tomography and ultrasonography in the diagnosis of equivocal acute appendicitis. A meta-analysis. Saudi Med J. 2007 Feb;28(2):173-80. PMID: 17268692.
- Unlüer EE1, Yavaşi O, Eroğlu O, et al. Ultrasonography by emergency medicine and radiology residents for the diagnosis of small bowel obstruction. Eur J Emerg Med. 2010 Oct;17(5):260-4.)
- Taylor MR, Lalani N. Adult small bowel obstruction. Acad Emerg Med. 2013 Jun;20(6):528-44. doi: 10.1111/acem.12150. PMID: 23758299.
- Edwards, E.A., Pigg, N., Courtier, J. et al. Intussusception: past, present and future. Pediatr Radiol 47, 1101–1108 (2017). https://0-doi-org.catalog.llu.edu/10.1007/s00247-017-3878-x
- Tanner TN, Hall BR, Oran J. Pneumoperitoneum. Surg Clin North Am. 2018 Oct;98(5):915-932. doi: 10.1016/j.suc.2018.06.004. PMID: 30243453.
- Indiran, V., Kumar, R. V., & Jefferson, B. (2018, May 3). Enhanced peritoneal stripe sign. Abdominal Radiology, 43, 3518-3519.





[…] The Abdomen can be a black box Black large square when making diagnoses. Let #POCUS make your life e… […]