Primary Authors: Jade Deschamps, Vi Dinh; Co-authors: Jessica Ahn, Satchel Genobaga, Annalise Lang, Victor Lee, Reed Krause, Devin Tooma, Seth White. Oversight, Review, and Final Edits by Vi Dinh (POCUS 101 Editor).
Renal ultrasound provides a fast, cost-effective, and radiation-free alternative to CT scans for the initial workup of patients with renal complaints.
In this post we will show you how to use Point of Care Ultrasound to:
- Perform Renal Ultrasound in a Step-by-Step Protocol
- Easily Grade Hydronephrosis
- Evaluate for Renal/Kidney Stones with Ultrasound vs CT Scan
- Evaluate other Renal Ultrasound Pathology (Renal Cysts and Masses)
- Perform Renal Hemodynamics (Renal Resistive Index and Intrarenal Venous Doppler)
We also made a Renal Ultrasound Hydronephrosis Grading PDF Pocket card you can download as a reference!
Table of Contents
Hydronephrosis POCKET CARD PDF
One of the most common reasons to perform POCUS is to evaluate for hydronephrosis. So we made a Free Renal Ultrasound PDF Pocket card below to easily grade Hydronephrosis! Just click to download!
Renal Ultrasound Indications
- Unilateral flank pain, low back pain, lower abdominal pain, or groin pain
- Undifferentiated abdominal, flank, groin, or genital pain
- Dysuria (pain with urination)
- Hematuria
- Anuria or Oliguria (decreased urinary output)
- Urinary incontinence or problems voiding
Renal Ultrasound Preparation
Patient Preparation
- The patient will lie supine.
- If you are having difficulty getting views you can have the patient sit up and scan posteriorly or have them lay in the left/right lateral decubitus positions.
Ultrasound Machine Preparation
- Transducer: Curvilinear Ultrasound Probe or Phased Array Probe.
- Preset: Abdominal or Renal
- Machine Placement: Place the machine on the patient’s right side so you can scan with your right hand and manipulate ultrasound buttons with your left hand.

Kidney/Renal Ultrasound Anatomy
The urinary system is composed of the kidneys, ureters, bladder, and urethra, which work together to maintain the fluid balance of the body and filter toxins from the blood. In this post we will focus on the kidneys, however, we created a separate post on bladder ultrasound which you can access HERE.
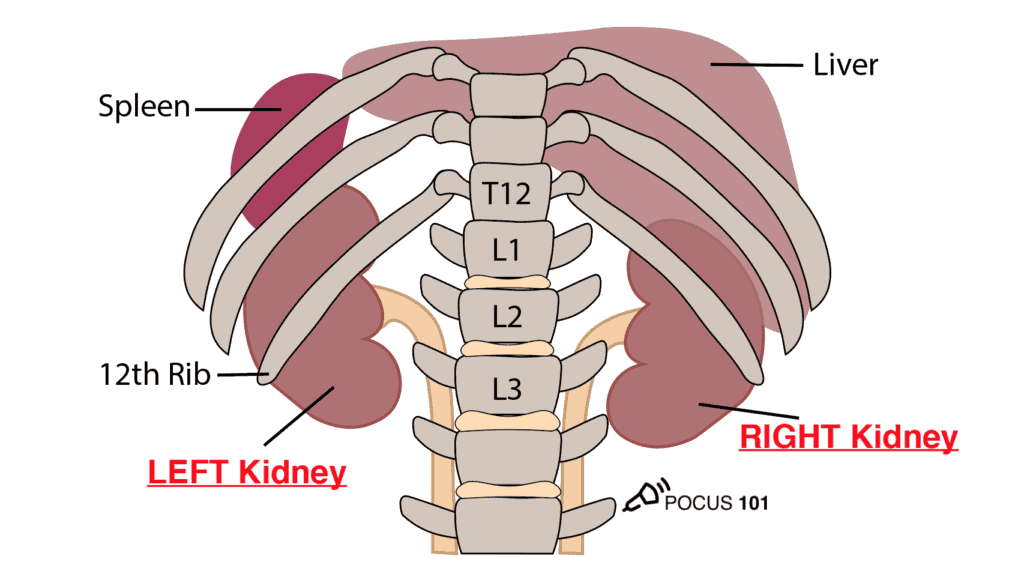
The kidneys are retroperitoneal organs located on either side of the vertebral column from T12-L3. Notice that the right kidney is slightly more posterior than the left kidney because of the larger size of the liver relative to the spleen.
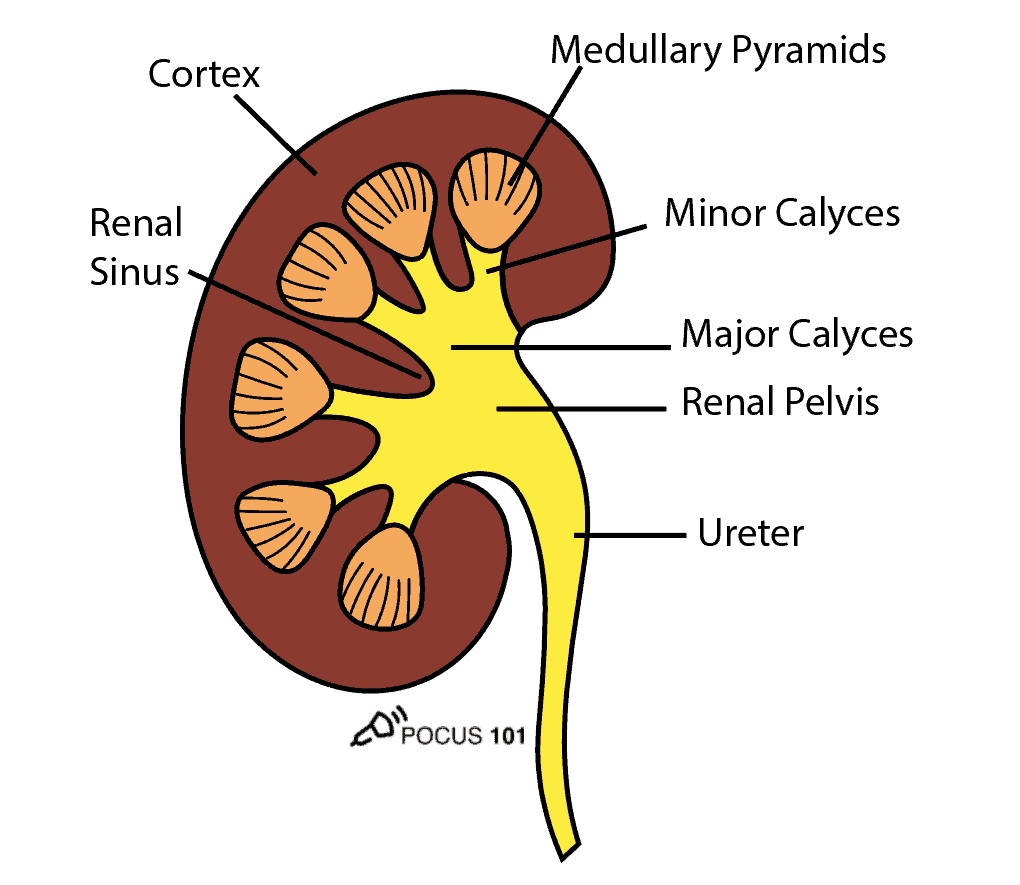
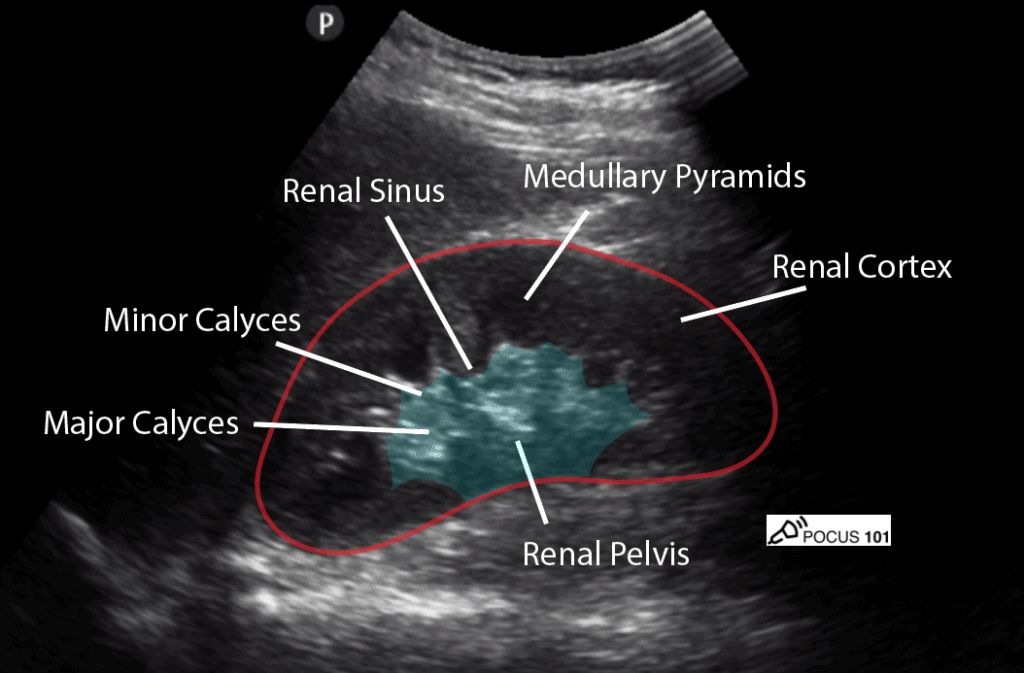
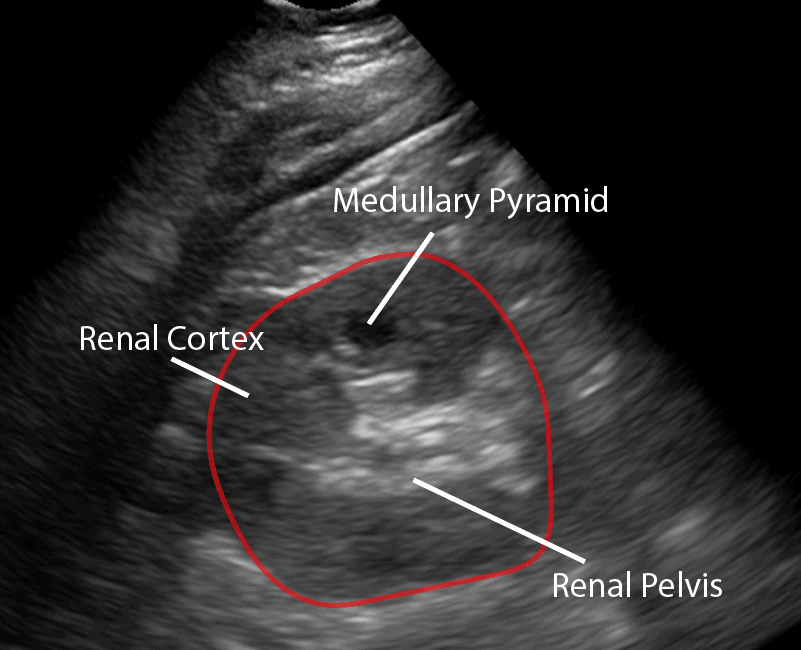
To perform renal ultrasound here are the key renal anatomic structures you should know:
- Renal Cortex
- Medullary Pyramids
- Minor Calyces
- Major Calyces
- Renal Pelvis
- Renal Sinus
POCUS 101 Tip: Remember, renal and bladder scans should often be done together because they are often implicated together in renal pathology. We made a separate post for scanning the Bladder which you can find HERE.
Step-by-Step Renal Ultrasound Protocol
We will scan both the left and right kidneys using the long-axis and short-axis, also known as longitudinal and transverse views.
Step 1: RIGHT Kidney Ultrasound Longitudinal View
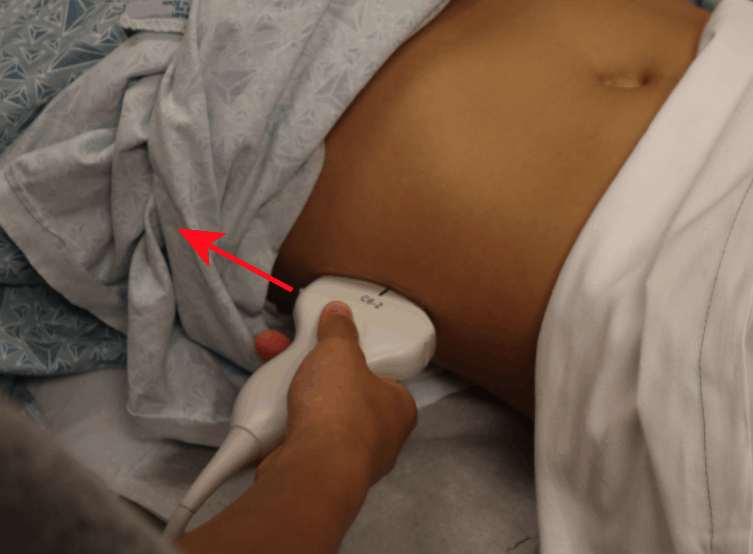
- Point the probe indicator towards the patient’s head.
- Place your probe at the Right Midaxillary Line around the 10th to 11th intercostal space.
- POCUS 101 Tip: You may need to rotate the transducer 10-20 degrees counter-clockwise to get in between the rib spaces and optimize your view.
- Center the kidney on the ultrasound screen.
- Identify the: Liver, Renal Cortex, Medullary Pyramids, Renal Pelvis, Renal Sinus, Mainor Calyces, Minor Calyces.
- The normal size of an adult kidney is around 10-11cm in the longitudinal view.
- Slowly tilt/fan the probe anteriorly and posteriorly to assess the entire kidney.
Step 2: RIGHT Kidney Ultrasound Transverse View
- Maintaining the longitudinal view of the right kidney, center the kidney on your screen, and then rotate your probe 90 degrees counterclockwise.
- The probe indicator should be pointing Posteriorly.

- Here is the ultrasound image transition that you should see as you go from the longitudinal kidney ultrasound view to the transverse view.
- In the transverse view, identify the Renal Cortex, Medullary Pyramid, and Renal Pelvis.
- Tilt the probe superiorly and inferiorly to assess the right kidney.
Step 3: LEFT Kidney Ultrasound Longitudinal View
The technique for scanning the left kidney is very similar to that of the right kidney. Of note, the left kidney lies slightly superior and posterior compared to the right kidney due to the smaller size of the spleen.
- Point the probe indicator towards the patient’s head.
- Place your probe at the Left Posterior Axillary Line around the 8th to 10th intercostal space.
- To reach the posterior axillary line, your knuckles should touch the bed.
- Visualize the same renal structures you did in the Right Kidney (except instead of the liver you will see the spleen above the left kidney in this view).
- POCUS 101 Tip: Sometimes you may need to rely on the patient’s breathing pattern to bring the left kidney into view.

Step 4: LEFT Kidney Ultrasound Transverse View
- Maintaining the longitudinal view, center the kidney on your screen, and then rotate your probe 90 degrees counterclockwise.
- The indicator should be pointing Anteriorly.
- Tilt the probe superiorly and inferiorly to assess the entire left kidney.
- Visualize the same renal structures you did in the Right Kidney.

Renal Ultrasound Pathology
Hydronephrosis, kidney stones, renal cysts, and masses are all detectable with ultrasound. Here, we will explain the key findings and clinical presentations of these common conditions.
Hydronephrosis Ultrasound Grading
Hydronephrosis is defined as abnormal enlargement and distension of a kidney caused by obstructive uropathy (blockage of normal urine flow into the ureter). Patients may present with varying symptoms depending on the causes of hydronephrosis.
Here are some of the most common causes of hydronephrosis and obstructive uropathy:
- Kidney Stones
- Bladder Stones
- Benign Prostatic Hyperplasia (BPH)
- Cancer (bladder, renal, uterine, colon, cervical)
- Dysfunctional Bladder (urinary retention)
Evaluating for Hydronephrosis with renal ultrasound is one of the most common Point of Care Ultrasound (POCUS) applications. Thankfully POCUS is easy to perform/interpret while being very sensitive and specific for diagnosing hydronephrosis.
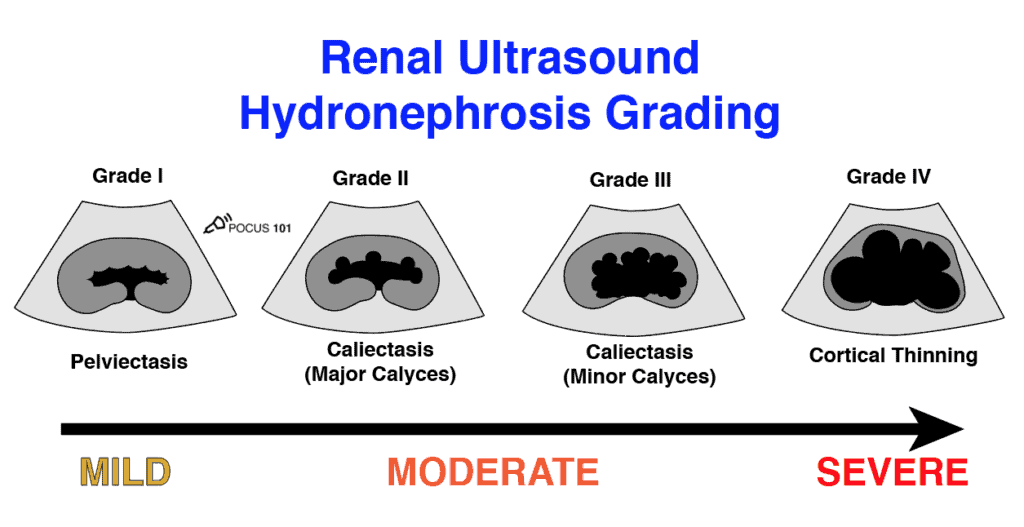
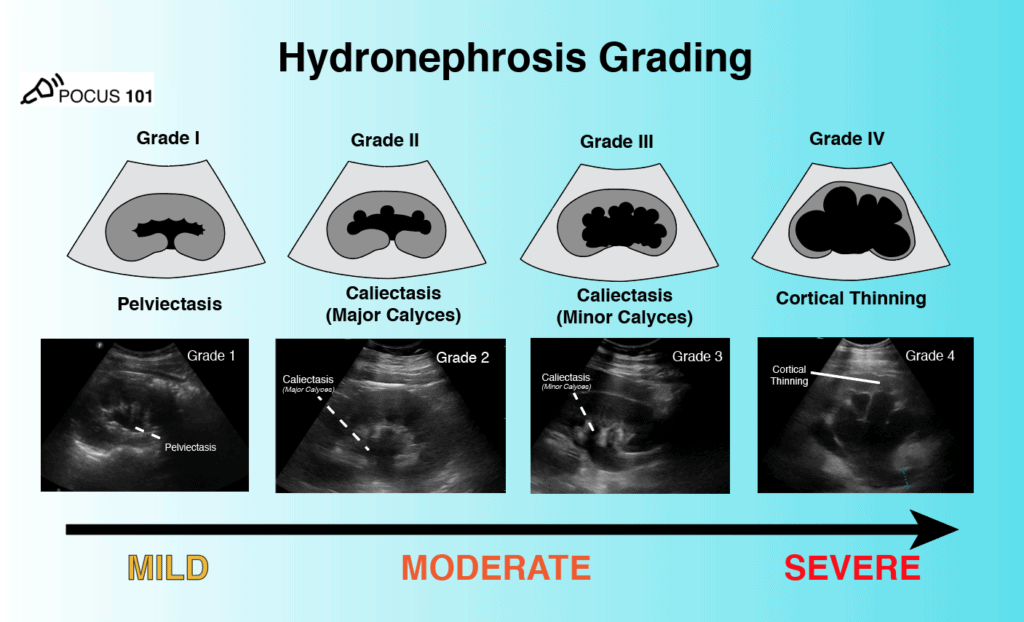
Initially, it may seem confusing or hard to memorize all of the terms to grade hydronephrosis using ultrasound. However, hydronephrosis grading is actually very simple!
POCUS 101 Tip: Don’t memorize the hydronephrosis grading system, just think that the structures closest to the obstruction will be the first to be dilated. So the order of hydronephrosis will be Renal Pelvis -> Major Calyces -> Minor Calyces -> Renal Cortex. Using this method, you can derive the entire hydronephrosis grading system.

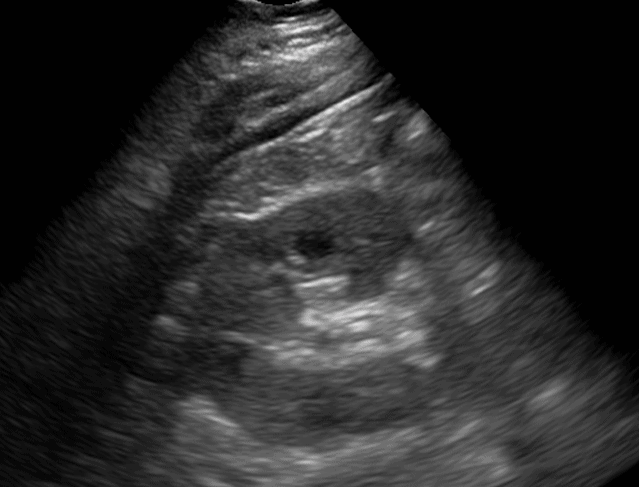
Now there are few different ways to grade hydronephrosis. The simplest way is to grade hydronephrosis as Mild, Moderate, or Severe. The other way, which you may see in radiology reports, is to use a 1-4 hydronephrosis grading system with descriptions of the hydronephrosis findings (i.e. peviectasis, caliectasis, cortical thinning). The figure below sums up the most commonly used hydronephrosis grading systems.
Grade 0 Hydronephrosis – Normal
Sometimes you may see the term “Grade 0” Hydronephrosis. Don’t worry there isn’t any actual hydronephrosis, that just means that the kidney appears normal!
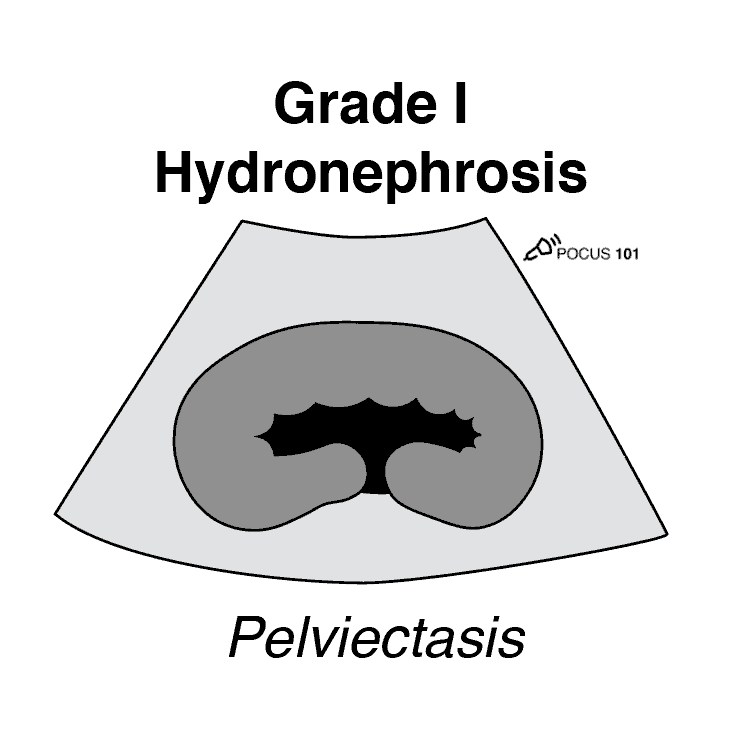
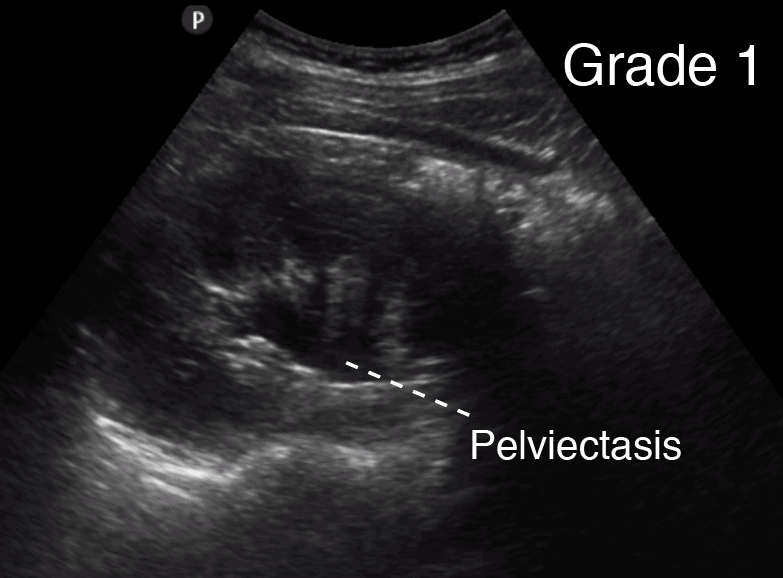
Grade 1 Hydronephrosis (Mild)
Grade 1 Hydronephrosis or “Mild” Hydronephrosis occurs when there is dilatation of the renal pelvis (Pelviectasis) without dilatation of the calyces. The renal cortex (parenchyma) is preserved and does not show any atrophy.
Editor’s Note: Grade 1 Hydronephrosis (Pelviectasis) can be found in healthy/normal patients that have not voided for a prolonged amount of time. Make sure to have the patient void prior to the renal ultrasound exam to accurately access for hydronephrosis.
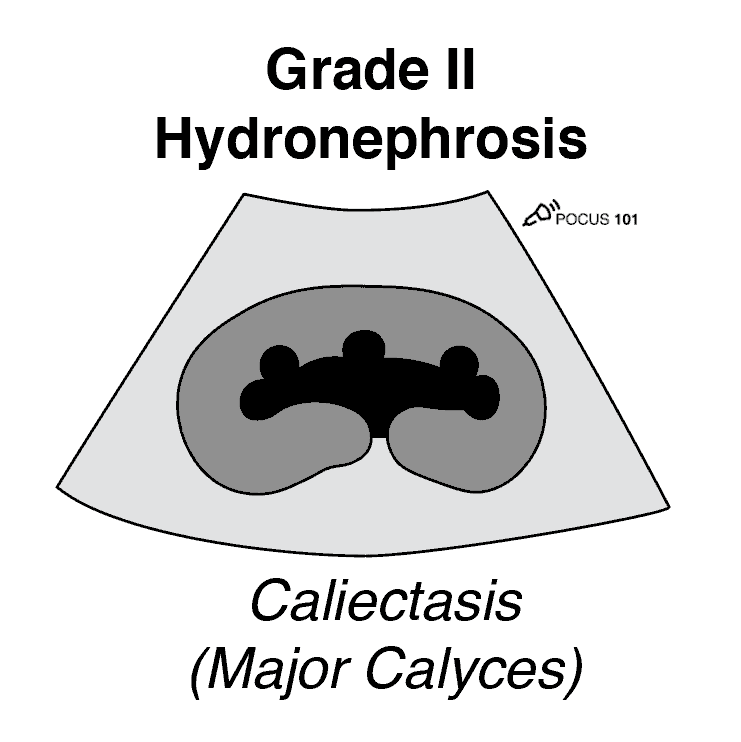
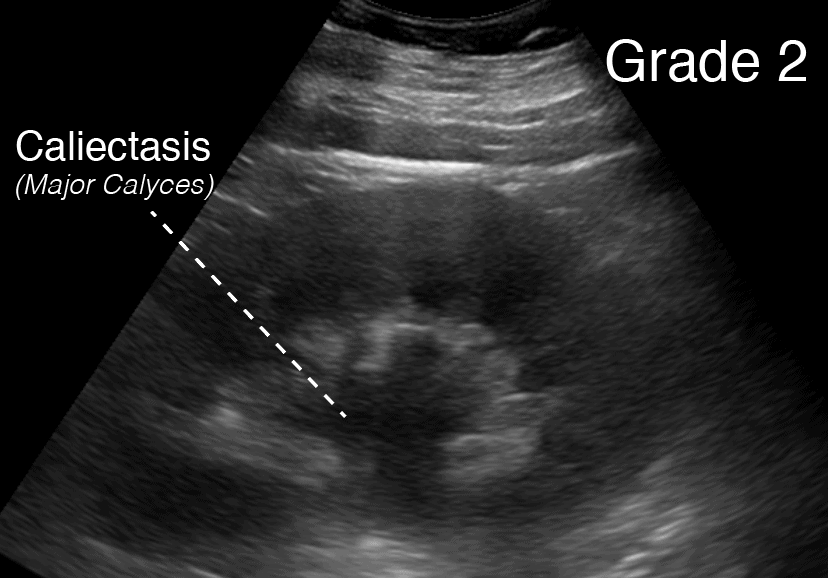
Grade 2 Hydronephrosis (Mild-Moderate)
Grade 2 Hydronephrosis or “Mild-Moderate” Hydronephrosis occurs when you have dilatation of the renal pelvis (Pelviectasis) and dilatation of the Calcyces (Caliectasis), specifically the MAJOR Calyces. The renal cortex (parenchyma) is preserved and does not show any atrophy.
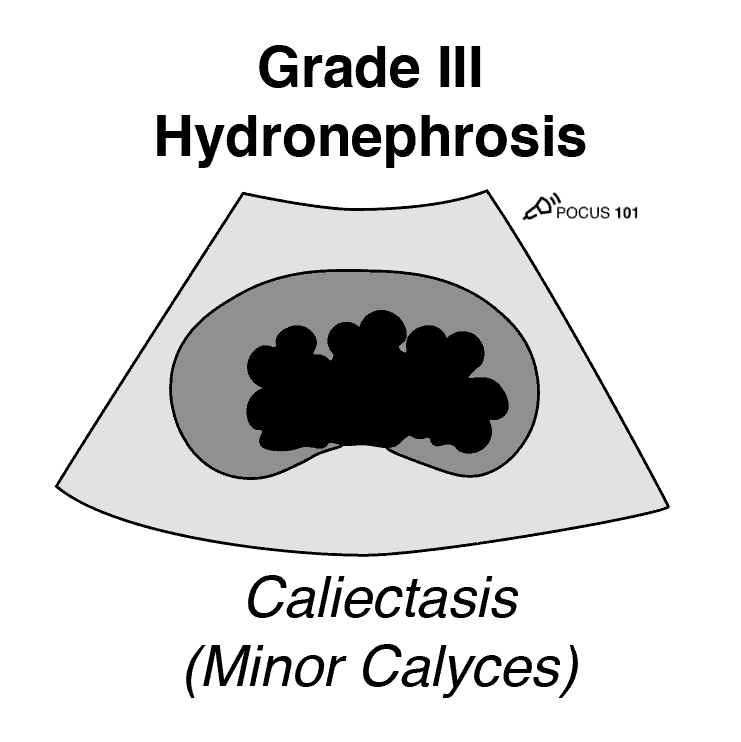
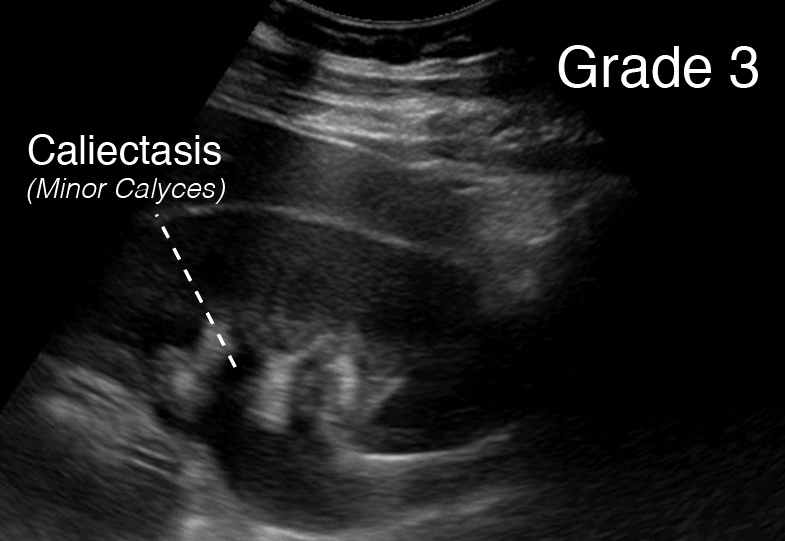
Hydronephrosis Grade 3 (Moderate)
Grade 3 Hydronephrosis or “Moderate” Hydronephrosis occurs when you have dilatation of the renal pelvis (Pelviectasis) and dilatation of the Calcyces (Caliectasis), specifically the MAJOR and MINOR Calyces. Mild cortical thinning may be seen.
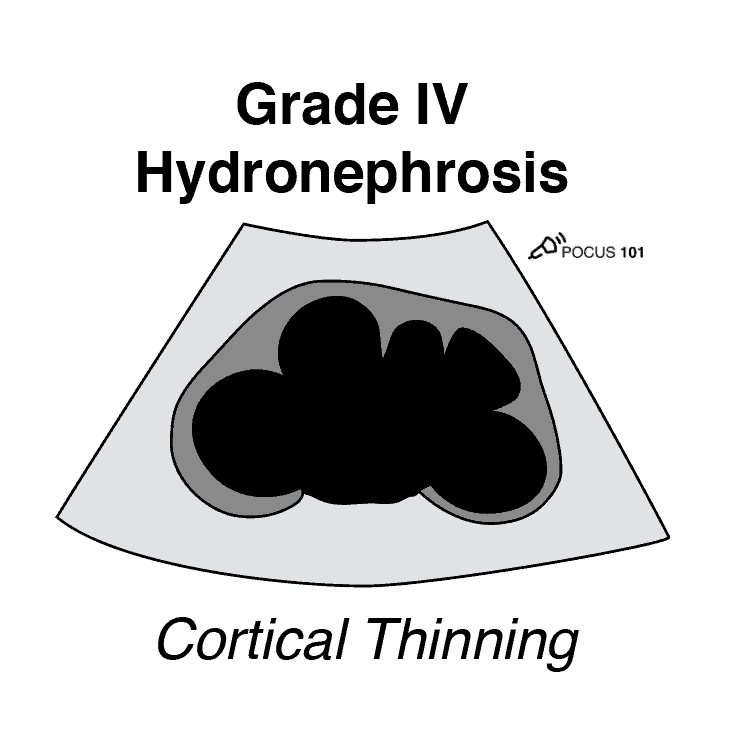
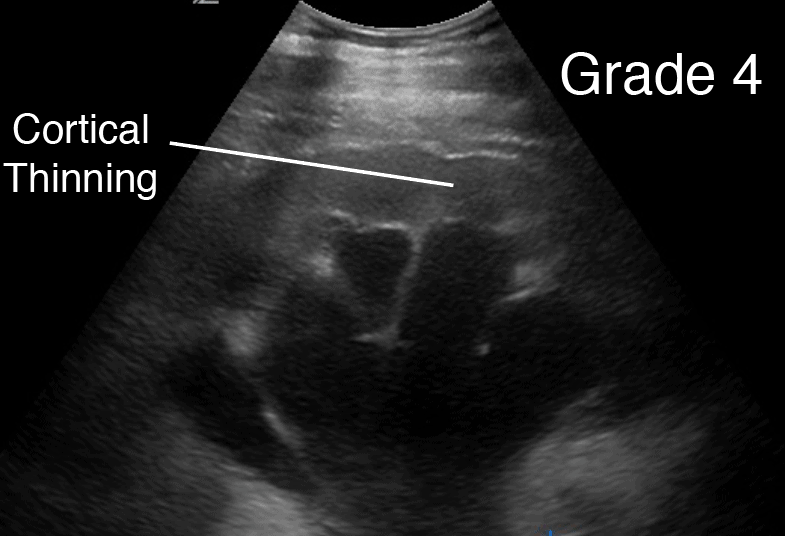
Hydronephrosis Grade 4 (Severe)
Grade 4 Hydronephrosis or “Severe” Hydronephrosis occurs when there is significant/gross dilatation of the renal pelvis (Pelviectasis) and Calcyces (Caliectasis) resulting in renal cortical thinning. There will also be renal atrophy and loss of the borders between the renal pelvis and calyces. Grade 4 hydronephrosis is also sometimes called the “Bear Claw” Sign since the anechoic areas resemble a paw print.
Don’t forget to download the Hydronephrosis Ultrasound Grading PDF Pocket Guide!
Hydronephrosis Mimics
Hydronephrosis Mimics can present as false positives for true hydronephrosis.
Here are some of the most common causes of Hydronephrosis Mimics:
- Extrarenal Pelvis
- Parapelvic Cysts
- Vascular Malformation
The images below are from @NephroP. For more information on in-depth details on hydronephrosis mimics, we recommend visiting nephropocus.com!
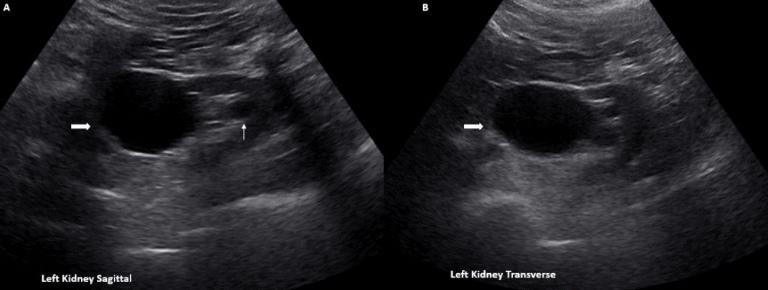
Extrarenal Pelvis
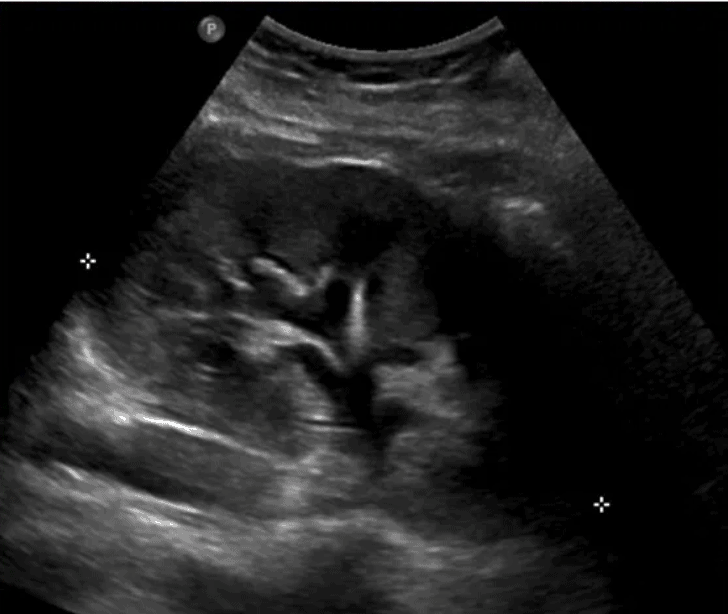
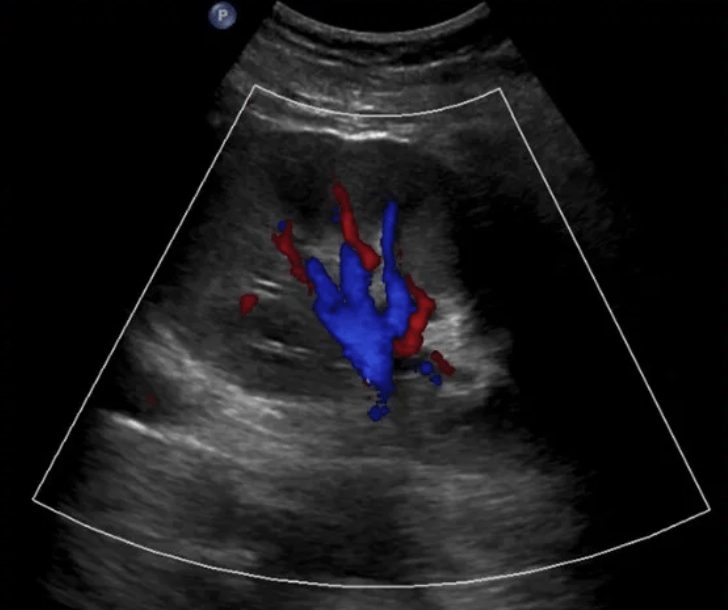
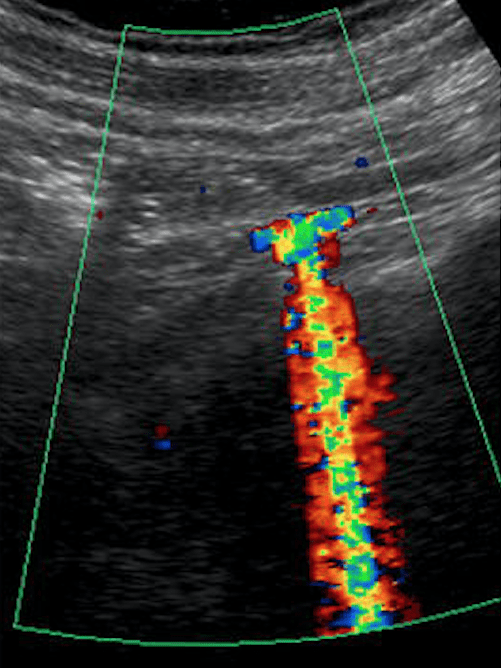
An extrarenal pelvis is a normal and often benign anatomical variant that lies predominantly outside the renal sinus. Regarding extrarenal pelvis vs hydronephrosis, an extrarenal pelvis on ultrasound will appear as an anechoic structure adjacent to the renal sinus without any pelviectesis, caliectasis, or cortical thinning. You can also place color Doppler on it to make sure there is no arterial/venous flow present.
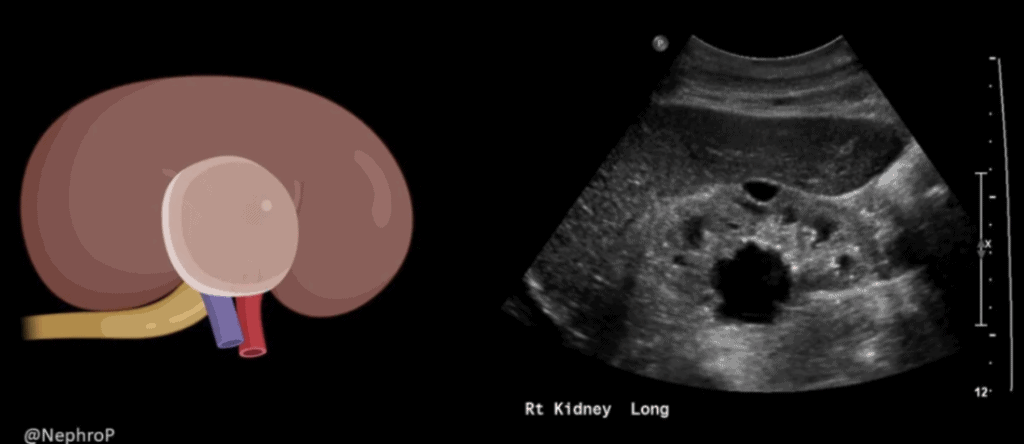
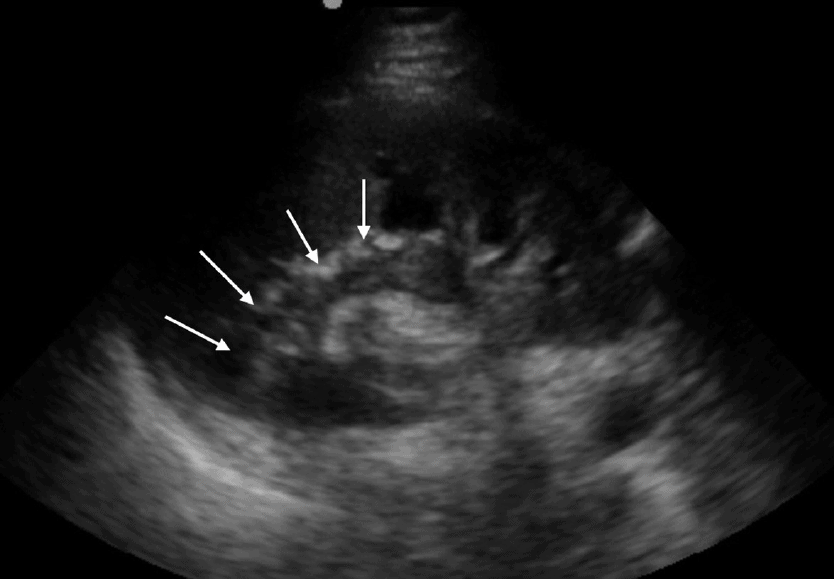
Parapelvic Cyst
A parapelvic cyst is a cyst that forms near the renal pelvis. They are normally painless unless they grow too large and compress the kidney. Though they are associated with a history of urinary obstruction, the cyst itself rarely causes any obstruction (Koratala 2018).
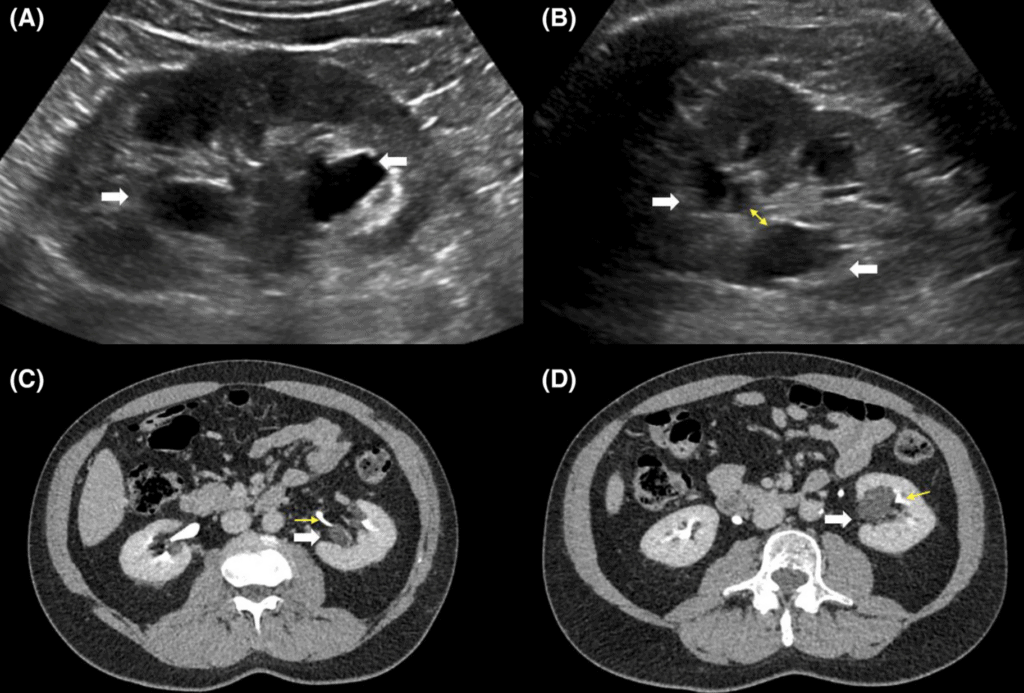
Prominent Renal Vasculature and Vascular Malformation
Prominent renal arteries/veins and Renal Vascular Malformations (Abnormal communication between renal arteries and veins) can also cause false positives for hydronephrosis. Color Doppler indicates blood flow and can distinguish renal prominent vessels or vascular malformations from hydronephrosis (Bates, 2010).
Ureteral/Kidney Stones (Nephrolithiasis)
Kidney stones (also known as nephrolithiasis, urolithiasis, ureteral stone, renal stone, or renal calculi) result because of stony secretions in the bladder or urinary tract.
According to the National Kidney and Urologic Diseases Information Clearing House, more than half a million people visit emergency rooms, and nearly three million people visit their health care provider, for problems with kidney stones.
These patients classically present with:
- Severe pain in their abdomen, groin, genitals, or flank
- Fever and chills
- Severe nausea or vomiting
- Hematuria
Kidney Stone Size
The cutoff size for a significant kidney stone size is around 5mm. Stones <5mm have a significantly higher chance (81-98%) of spontaneously passing while stones >5mm will have an exponentially lower chance (9-65%) of spontaneously passing (Jendeberg 2010). See the table below for spontaneous passage rates for specific ureteral stone sizes.
| Ureteral Stone Size | Spontaneous Passage % |
| 0-2mm | 98% |
| 3mm | 98% |
| 4mm | 81% |
| 5mm | 65% |
| 6mm | 33% |
| >6.5mm | 9% |
Kidney Stone Location
Kidney stones may be located within the renal parenchyma, at the ureteropelvic junction (between the ureter and the renal pelvis), within the ureter, or at the ureterovesical junction (between the ureter and the bladder).
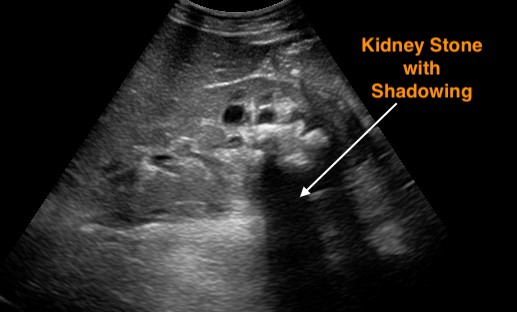
Ultrasound Findings for Kidney Stones:
There are multiple ways to look for the presence of kidney stones on ultrasound. The ultrasound findings you see will depend on the size/location of the kidney stone and the amount of obstruction.
Here are some of the more commonly described ultrasound findings for kidney stones:
- Direct Visualization of Stone
- Hydronephrosis of affected kidney
- Absence of Ureteral Jets
- Twinkling Artifact
1. Direct Ultrasound Visualization of Kidney Stone
The most definitive way to see a kidney stone on ultrasound is by direct visualization. Unfortunately, this is a rare occurrence since most kidney stones lie in the ureter or the ureterovesical junction. With surrounding bowel gas it is difficult to directly visualize the bladder.
Sometimes renal stones can be seen in the renal cortex, pelvis, or the ureteropelvic junction. Look for a hyperechoic structure with Acoustic Shadowing.
2. Hydronephrosis of Affected Kidney
An indirect sign of obstructive uropathy from a kidney stone is to look for hydronephrosis on renal ultrasound. (Go to the previous section on how to use renal ultrasound to diagnose hydronephrosis)
A misconception is that the absence of hydronephrosis on renal ultrasound rules out a kidney stone. This isn’t true. If a kidney stone is small, it may still cause symptoms and renal colic without dilating the kidney.
While not 100% specific, there is evidence that patients with none or mild hydronephrosis on ultrasound are significantly more likely to have ureteral stones <5 mm and will likely pass them without the need for surgical intervention (Goertz 2010).
3. Absence of Ureteral Jets
Urine flows from the kidney, through the ureters, and finally enters the bladder at the trigone. Ultrasound “Ureteral Jets” are a color Doppler finding during bladder ultrasound that detects the flow of urine into the bladder at the level of the trigone.
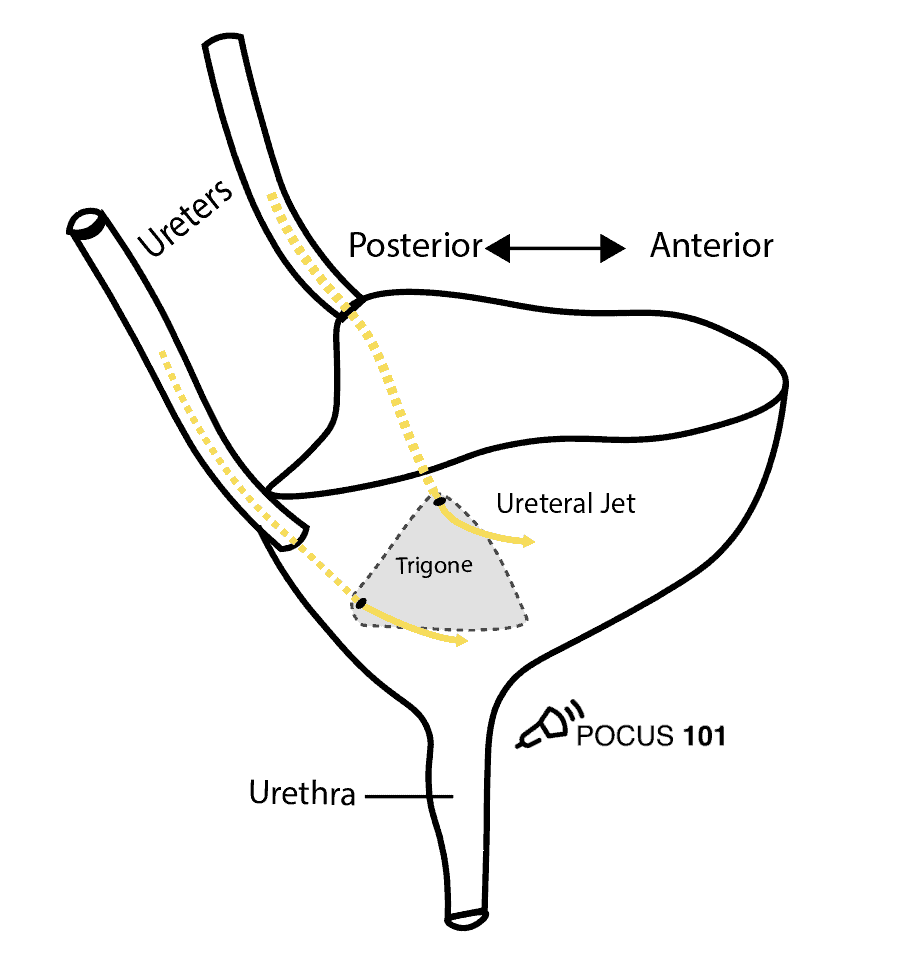
To evaluate for ureteral jets properly make sure you are in the transverse view of the bladder and decrease your color Doppler scale to about 10-20cm/s or you can use power Doppler. Urine is not continuously released into the bladder, and actually occurs at regular intervals. Therefore, you may need to wait up to 5-10 minutes to see if there are any ureteral jets.
If a suspected kidney stone is lodged within the ureter or ureterovesical junction, you may find an absence of ureteral jets on the obstructed side when scanning the bladder.
Here are examples of ultrasound ureteral jets from the right and left kidneys:
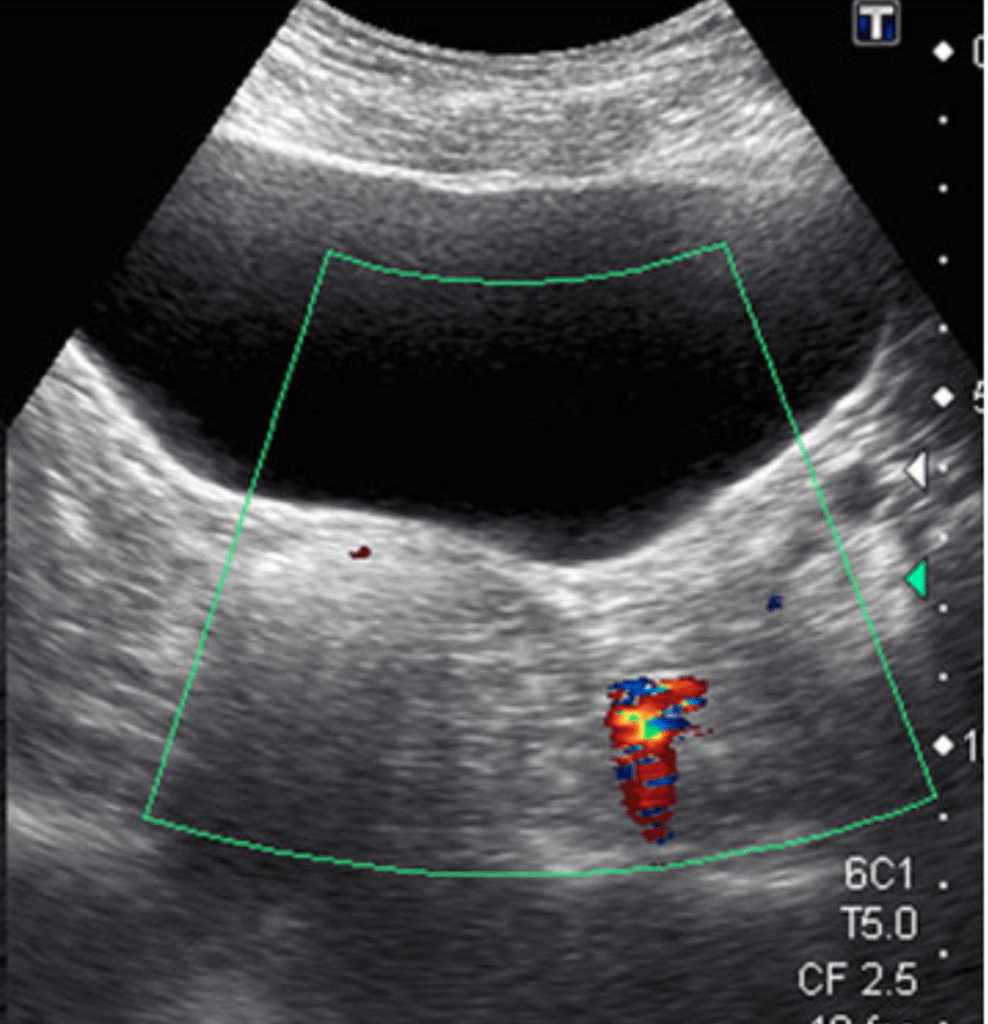
4. Twinkling Artifact
The Twinkling Artifact is a sonographic artifact located behind calcifications of ureteral calculi when color Doppler is applied. It will appear as a multicolored high-intensity signal, similar to signals produced by turbulent flow with aliasing.
This artifact may also be associated with a color comet-tail artifact, which, similar to a greyscale comet-tail artifact, occurs when an ultrasound beam encounters 2 strong parallel reflectors. This leads to the “tail” like appearance from numerous reverberation signals that the transducer is receiving.
The twinkling artifact has a sensitivity and specificity of 90% and 100%, respectively, for kidney stone at the ureterovesical junction (Ripollés 2013).
Ultrasound vs CT Scans for Kidney Stone Workup
A landmark study published in 2014 by the New England Journal of Medicine conducted at 15 various emergency departments evaluated the accuracy of Point of Care Ultrasound (POCUS) versus computed tomography (CT) scan as the initial imaging method for patients with suspected kidney stones. (Smith-Bindman et al, 2014)
The authors found that there was NO significant difference between POCUS and CT scans with regards to the following:
- Diagnostic accuracy
- Return emergency department visits or hospitalizations
- Incidence of high-risk diagnoses with complications
- Serious adverse events
- Average Pain score
The POCUS group however had a significantly lower amount of cumulative radiation exposure compared to the CT group.
This NEJM study concluded that Point of Care Ultrasound should be the first screening tool for patients with suspected kidney stones.
Editors Note: This is not to say that patients should only undergo ultrasound imaging, but rather the researchers advocate that it should be used as the initial diagnostic test. From there, it should be at the doctor’s discretion to order further imaging studies based on their clinical judgment.
Renal Cysts
Renal cysts are non-malignant, fluid-filled anechoic structures that are usually located in the parenchyma of the kidneys penetrating the cortex and medullary pyramids. They are common incidental POCUS findings and are usually benign and asymptomatic. (Bates, 2010)
Renal Cyst Ultrasound Findings
- Thin-walled and smooth, without septations or any internal elements.
- The anechoic areas of cysts are localized and do not connect to the calyces.
- Round or oval in shape
- Are located in the cortex or by the pelvis.
Editor’s Note: If these criteria are not fulfilled, you should consider a complex renal cyst, renal abscess, or malignancy that requires further workup. Also, make sure to differentiate kidney cysts from liver cysts by acquiring multiple ultrasound views.
PCKD and ARCD
If you see multiple renal cysts, this could indicate Polycystic Kidney Disease (PCKD) or acquired renal cystic disease (ARCD).
- Polycystic Kidney Disease (PCKD) is an inherited disorder that presents with an abundance of irregular renal cysts of varying size that distort the kidney’s shape bilaterally. Symptoms include flank pain, hematuria, hypertension, and renal failure.
- Acquired Renal Cystic Disease (ARCD) likewise presents with multiple kidney cysts but it is an acquired disorder and is seen in patients with end-stage renal disease on hemodialysis. It is associated with a higher risk of renal malignancy than PCKD.
Renal Masses
It is important to realize that not all focal hyperechoic lesions within the kidney are consistent with urolithiasis. A stone should have posterior acoustic shadowing. If a hyperechoic lesion with no acoustic shadow is seen within the kidney, you must consider a renal mass such as renal cell carcinoma (RCC) or angiomyolipoma (AML) (Forman 1993).
Renal masses can be detected incidentally during renal point of care ultrasound (POCUS). Any suspicious renal mass or abnormal kidney shape warrants referral to an expert and further workup (Sweeney, 1996).
Renal Cell Carcinoma (RCC)
- Most common Renal Malignancy in Adults.
- Highly variable with regards to size, shape, and location.
- Variable echogenicity: isoechoic, hypoechoic, or echoic
Angiomyolipoma
- Most common Benign Renal Tumor. (Tublin, 2011)
- Clearly circumscribed (i.e. angiomyolipoma) or irregular in shape (i.e. renal cell carcinoma).
- Often unilateral, but if bilateral, higher chance of malignancy.
- In some circumstances, renal cell carcinoma and angiomyolipoma can look very similar
Renal Hemodynamics
You can measure the renal arterial flow for renal resistive index or renal venous flow to assess for venous congestion. Both arterial and venous waveforms can give you significant information to predict Acute Kidney Injury (AKI) or to help limit venous congestion by limiting IV fluid administration.
The good news is that you can usually get the arterial AND venous waveforms in one tracing which we will show you exactly how to do below!
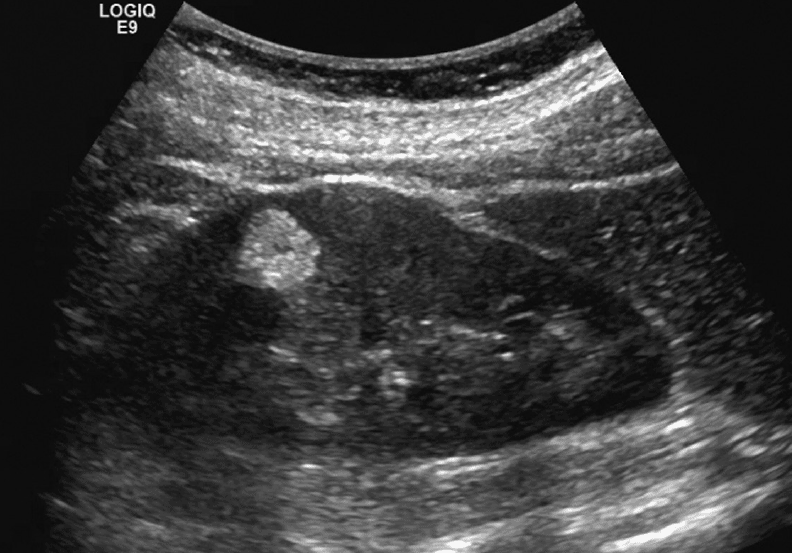
Step 1: Place Color Flow Doppler on the Kidney.
Editor’s Note: Make sure to decrease your color Doppler scale to about 12-25 cm/s and increase your color Doppler gain after as needed.
Step 2: Place pulse wave Doppler gate interlobar vessels and activate Doppler
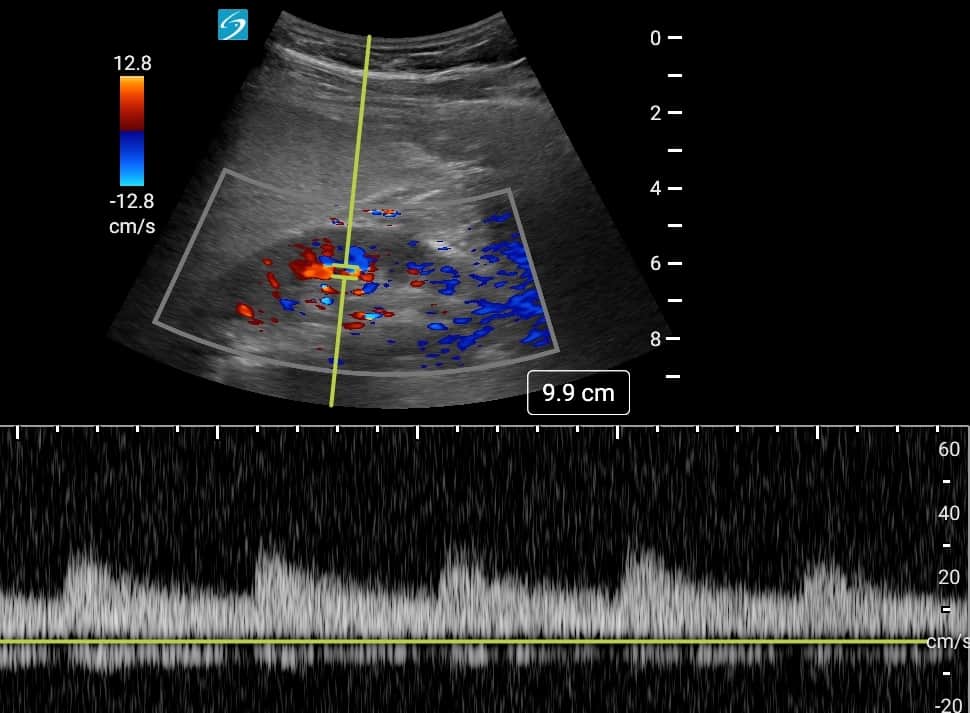
Here is a quick summary video on how to obtain the renal ultrasound color Doppler and pulse wave Doppler tracings:
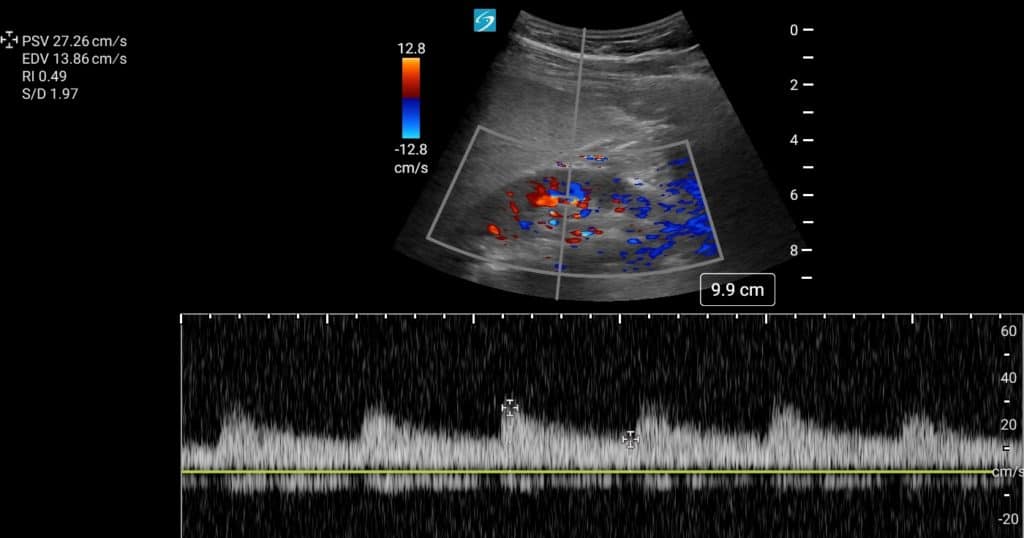
Renal Resistive Index (RRI)
The Renal Resistive Index is measured by placing the calipers at the Peak Systolic Velocity (PSV) and End Diastolic Velocity (EDV). A renal resistive index (RRI) of >0.7 is predictive of impending Acute Kidney Injury in multiple clinical settings including trauma and critical care (Song 2018).
The Renal Resistive Index is calculated using the following formula:
Renal Resistive Index Forumla: RRI = (PSV – EDV)/PSV
In the example below PSV = 27.26 cm/s and EDV = 13.86 cm/s
Therefore RRI = (27.26 cm/s – 13.86 cm/s) / 27.26 cm/s = 0.49
Renal Venous Congestion
Renal venous congestion can be evaluated by looking at the intrarenal venous Doppler tracings that occur below the baseline. For more indepth details, make sure to read our complete article on the VExUS ultrasound score to help you predict venous congestion.
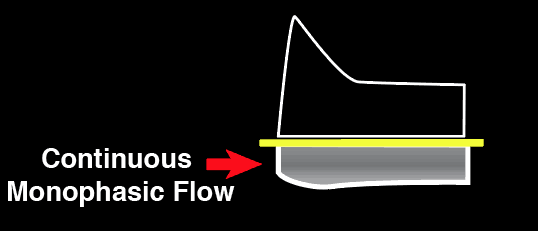
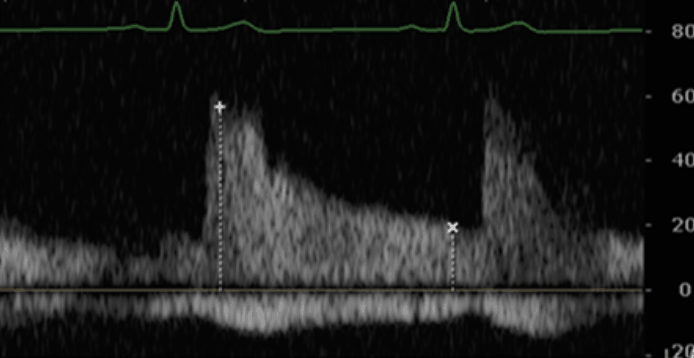
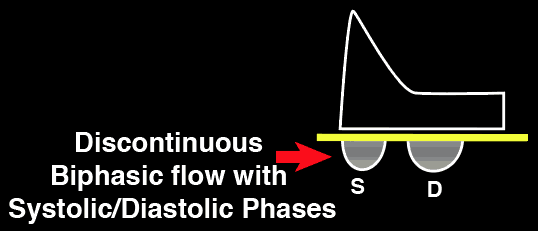
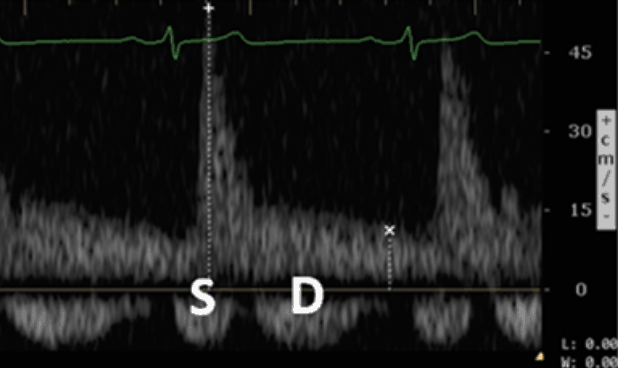
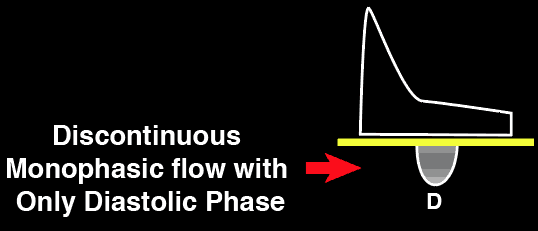
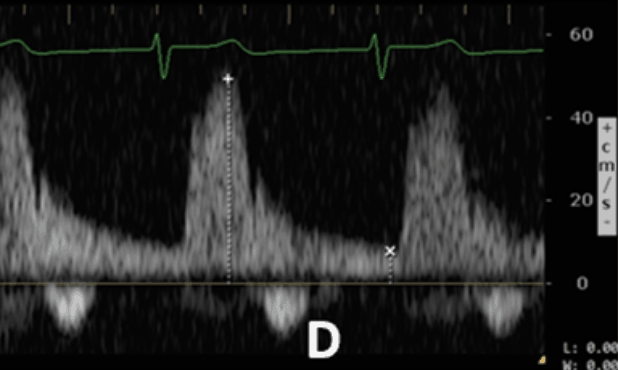
Below is a quick summary on how to interpret the intravenous venous Doppler tracings:
Normal Intrarenal Vein
Doppler
Mild Intrarenal Vein
Abnormality
Severe Intrarenal Vein
Abnormality
References
- Bates JA. Abdominal Ultrasound: How, Why and When. 3rd ed. New York, NY: Churchill Livingstone; 2010
- Nobel V, Brown DF. Renal ultrasound. Emerg Med Clin North Am. 2004;22:641-659
- Shukla, Amarnath. “The Ultrasound Mimics of Hydronephrosis.” Renal Fellow Network, 10 May 2019, www.renalfellow.org/2019/05/10/the-ultrasound-mimics-of-hydronephrosis/.
- Sim, Ki Choon. “Ultrasonography of Acute Flank Pain: a Focus on Renal Stones and Acute Pyelonephritis.” Ultrasonography, Korean Society of Ultrasound in Medicine, 26 Nov. 2017, www.e-ultrasonography.org/journal/view.php?doi=10.14366/usg.17051.
- Smith-Bindman, Rebecca, et al. “Ultrasonography versus Computed Tomography for Suspected Nephrolithiasis: NEJM.” New England Journal of Medicine, 18 Sept. 2014, www.nejm.org/doi/full/10.1056/NEJMoa1404446?query=featured_home#t=abstract.
- Staff, Science X. “Twinkle, Twinkle Kidney Stone: With a Push You Could Be Gone.” Medical Xpress – Medical Research Advances and Health News, Medical Xpress, 31 Jan. 2012, medicalxpress.com/news/2012-01-twinkle-kidney-stone.html.
- Sweeney, J., Thornhill, J., Grainger, R., Mcdermott, T., & Butler, M. (1996). Incidentally detected renal cell carcinoma: Pathological features, survival trends and implications for treatment. BJU International, 78(3), 351-353. doi:10.1046/j.1464-410x.1996.00140.x
- Tublin M, Thurston W, Wilson Sr. The kidney and Urinary tract. In: Rumack CM, Wilson SR, eds. Diagnostic Ultrasound. 4th ed. New York, NY: Elsevier; 2011
- “What Is a Renal Mass and What Is a Localized Renal Tumor?” Renal Mass and Localized Renal Tumors : Symptoms, Diagnosis & Treatment – Urology Care Foundation, www.urologyhealth.org/urologic-conditions/renal-mass-and-localized-renal-tumors.
- Koratala, A., Alquadan, K. (2018). Parapelvic cysts mimicking hydronephrosis Clinical Case Reports 6(4), 760-761. https://dx.doi.org/10.1002/ccr3.1431
- Jendeberg, J., Geijer, H., Alshamari, M., Cierzniak, B., Lidén, M. (2017). Size matters: The width and location of a ureteral stone accurately predict the chance of spontaneous passage. European radiology 27(11), 4775 – 4785. https://dx.doi.org/10.1007/s00330-017-4852-6
- Goertz, J., Lotterman, S. (2010). Can the degree of hydronephrosis on ultrasound predict kidney stone size? The American Journal of Emergency Medicine 28(7), 813 – 816. https://dx.doi.org/10.1016/j.ajem.2009.06.028
- Aytaç SK, Ozcan H. Effect of color Doppler system on the twinkling sign associated with urinary tract calculi. J Clin Ultrasound. 1999;27(8):433– 439.
- Ripollés T, Martínez- Pérez MJ, Vizuete J, Miralles S, Delgado F, Pastor- Navarro T. Sonographic diagnosis of symptomatic ureteral calculi: usefulness of the twinkling artifact. Abdom Imaging. 2013;38(4):863– 869.
- Tchelepi H, Ralls PW. Color comet-tail artifact: clinical applications. AJR Am J Roentgenol. 2009;192(1):11– 18.
- Forman HP, Middleton WD, Melson GL, McClennan BL. Hyperechoic renal cell carcinomas: increase in detection at US. Radiology. 1993;188(2):431– 434.
- Song, J., Wu, W., He, Y., Lin, S., Zhu, D., Zhong, M. (2018). Value of the combination of renal resistance index and central venous pressure in the early prediction of sepsis-induced acute kidney injury. Journal of Critical Care 45(), 204 – 208. https://dx.doi.org/10.1016/j.jcrc.2018.03.016
- Chiem A, Dinh VA. Emergency and Clinical Ultrasound Board Review. 1st Edition. Oxford 2020.




how to differentiate capillary leak affecting kidneys vs venous congestions as a cause of AKI as treatment is different using RENAL DOPPLER .