Primary Authors: Jade Deschamps, Vi Dinh; Co-authors: Jessica Ahn, Satchel Genobaga, Annalise Lang,Victor Lee, Reed Krause, Devin Tooma, Seth White. Oversight, Review, and Final Edits by Vi Dinh (POCUS 101 Editor).
One of the most important and underrecognized organs is the bladder. We assess it each day in our clinical practice using urine output, urinalysis, and physical exam. Even newer technology such as the “Verathon BladderScan” can significantly under or overestimate bladder volume from our experience.
Using Point of Care Ultrasound (POCUS) to evaluate the bladder is the easiest, quickest, and most accurate way to directly visualize the bladder at the bedside. Bladder ultrasound allows you to assess bladder volume, bladder obstruction, foley catheter placement/malfunctions, and other bladder pathology such as bladder stones, ureteral jets, and bladder masses.
In this post we will show you how to use Point of Care Bladder Ultrasound to:
- Perform Bladder Ultrasound in a Step-by-Step Fashion
- Measure Bladder Volume
- Recognize Common Bladder Ultrasound Pathology
Table of Contents
Bladder Ultrasound Indications
- Concern for postrenal acute kidney injury
- Voiding dysfunction
- Estimation of bladder volume (post-void residual)
- Hematuria
- Confirmation of proper urinary foley catheter placement
- Troubleshooting malfunctioning foley catheter
Patient and Machine Preparation
Patient Preparation
- The patient will lie supine. You may have the patient bend their knees to soften their abdominal wall.
- Since you will be scanning in the suprapubic region, make sure to place a towel or sheet to cover the patient’s pelvic area.
Ultrasound Machine Preparation
- Transducer: Curvilinear Ultrasound Probe or Phased Array Probe. Curvilinear is preferred because its wider footprint allows full visualization of the bladder.
- Preset: Abdominal or Renal
- Machine Placement: Place the machine on the patient’s right side so you can scan with your right hand and manipulate ultrasound buttons with your left hand.

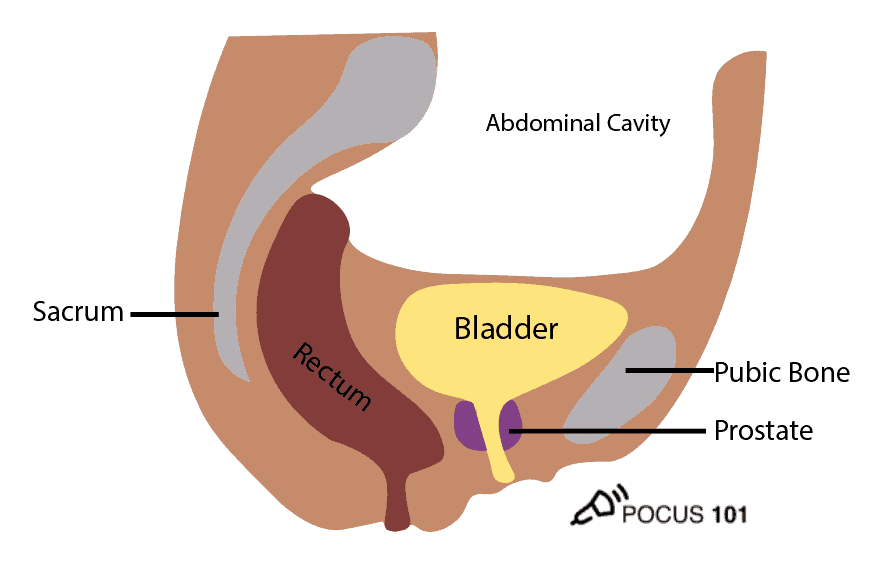
Bladder Anatomy
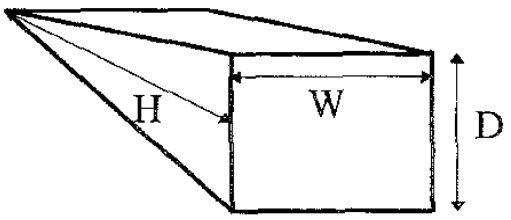
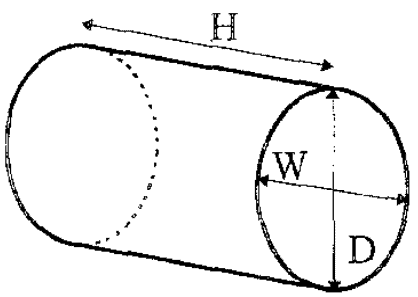
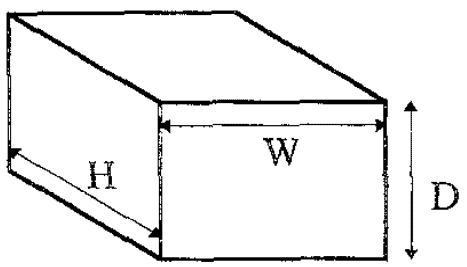
When starting to learn bladder ultrasound, figuring out the shape of the bladder can be confusing. Keep in mind that the shape of the bladder varies greatly depending on anatomical differences and how full the bladder is. Though it can be easy to think of the bladder as spherical in shape, in actuality it most often represents a shape of a triangular prism, cylinder (ellipsoid), or cuboid.
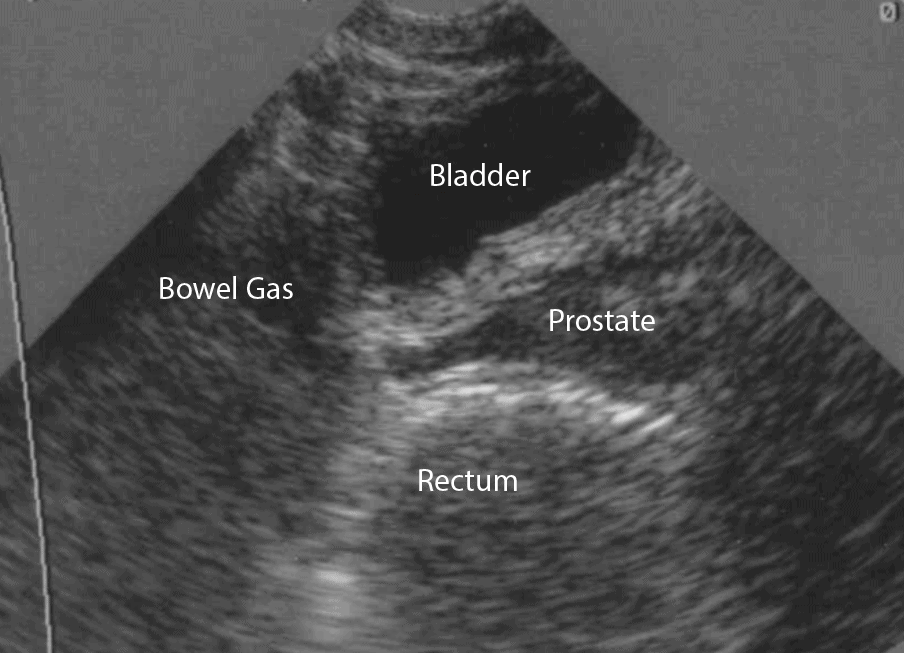
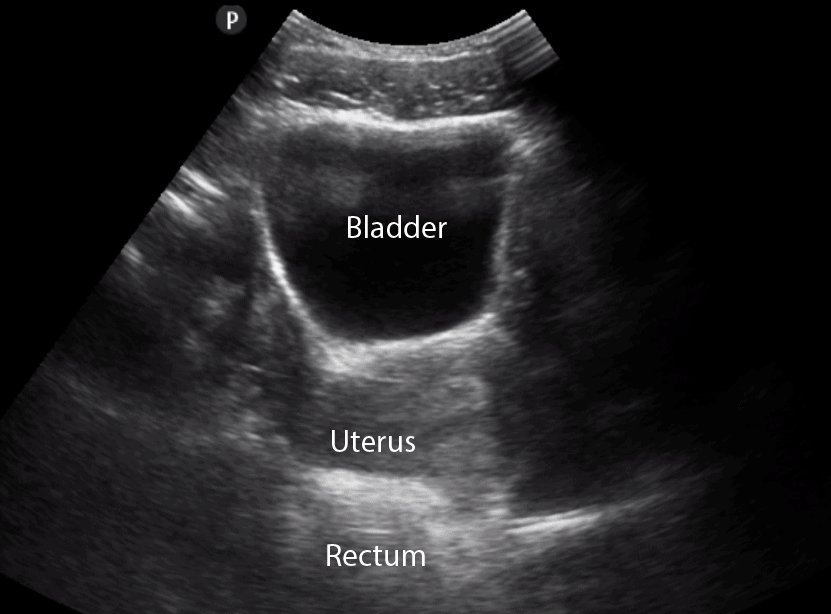
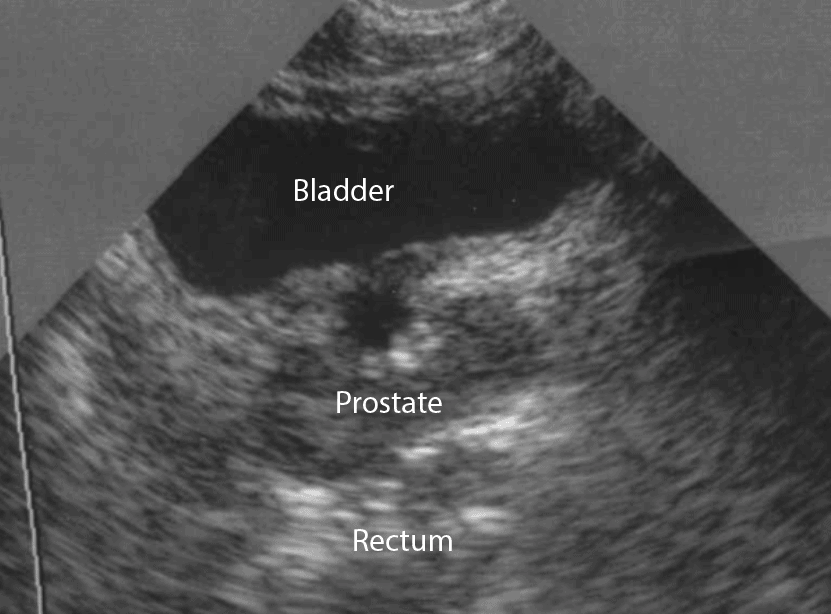
In addition to the bladder itself, it is also important to understand the surrounding structures including the pubic bone, abdominal cavity and rectum. The uterus and prostate are also important landmarks for females and males respectively.
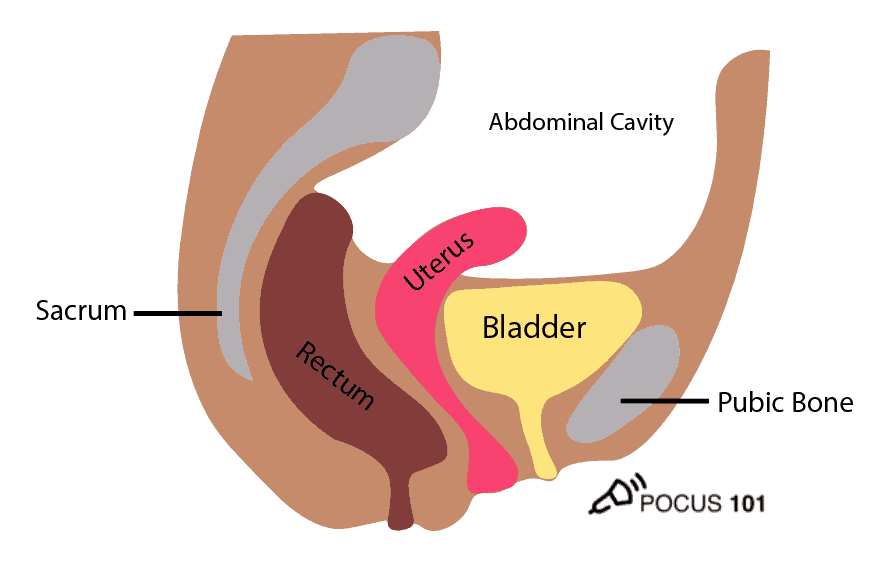
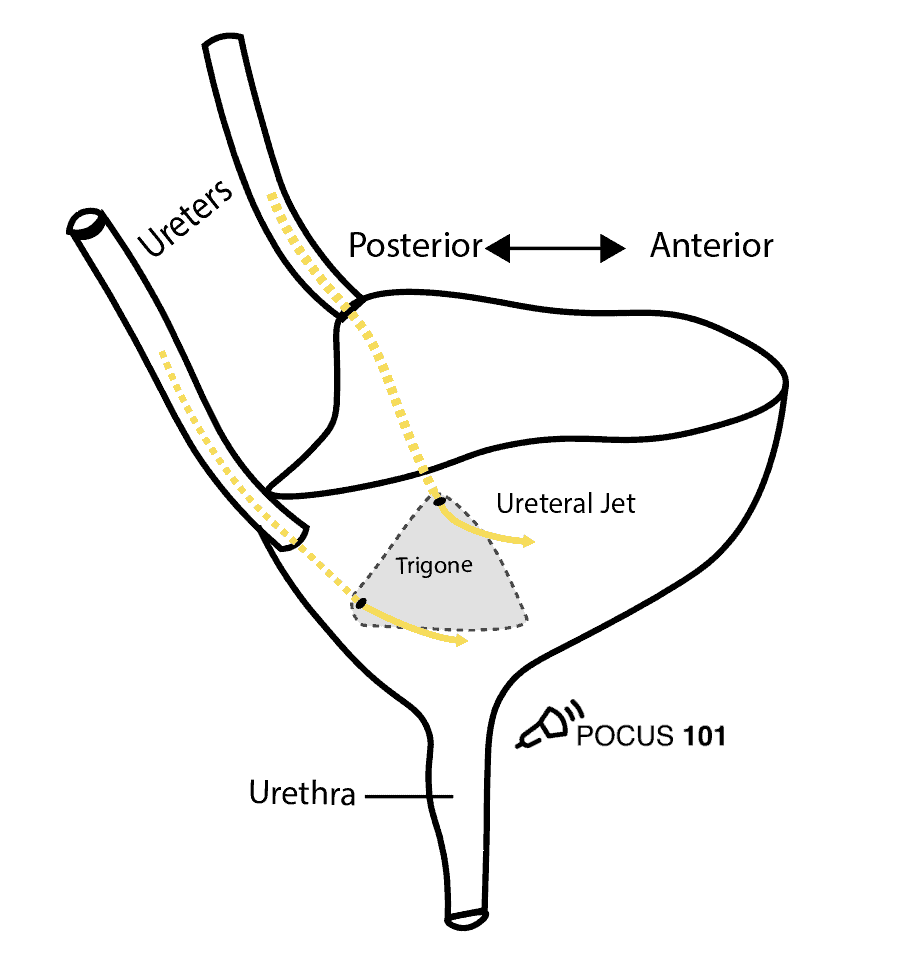
The ureters enter the top of the bladder but do not release urine until they reach the trigone of the bladder located inferiorly. This is important to know when you are evaluating “ureteral jets” on ultrasound.
Step-by-Step Bladder Ultrasound Protocol
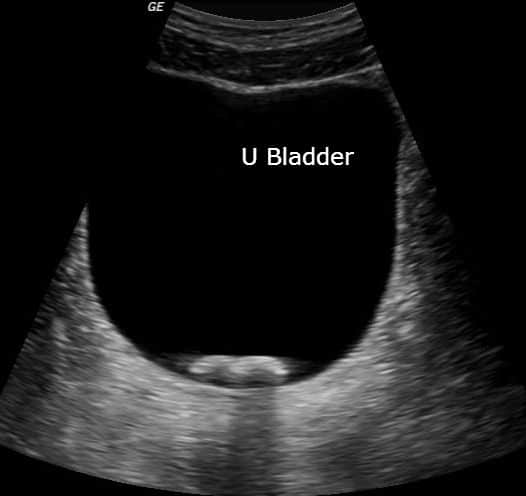
Step 1: Bladder Ultrasound – Longitudinal View
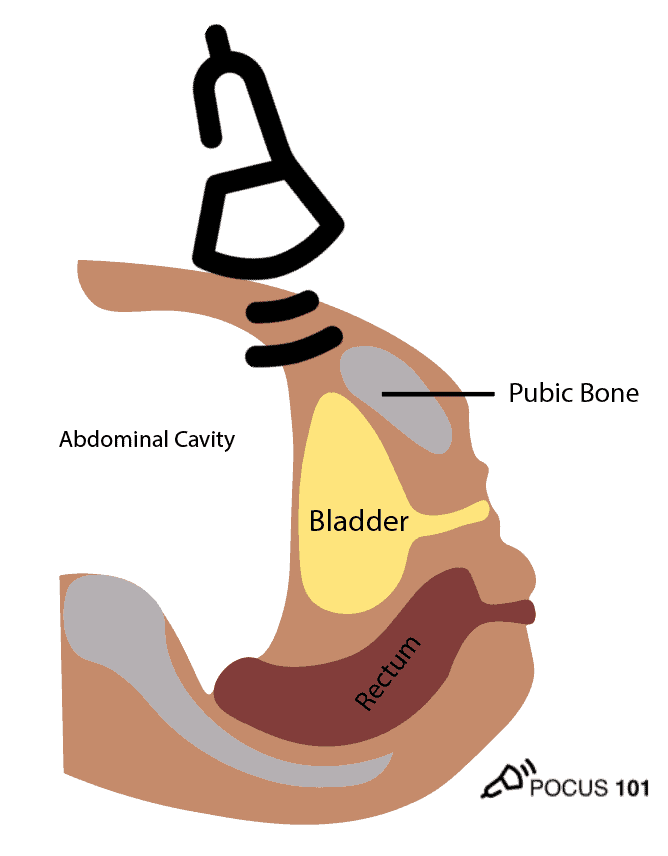
- Place the transducer with the indicator pointing towards the patient’s head in the patient’s midline, right above the pubic symphysis.
- Rock the probe so that it points down towards the pelvic cavity.

POCUS 101 Tip: One of the most important things to remember when performing bladder ultrasound is that the bladder is directly posterior to the pubic bone/symphysis. If you are unable to get proper images, most likely your ultrasound probe is placed too superiorly.
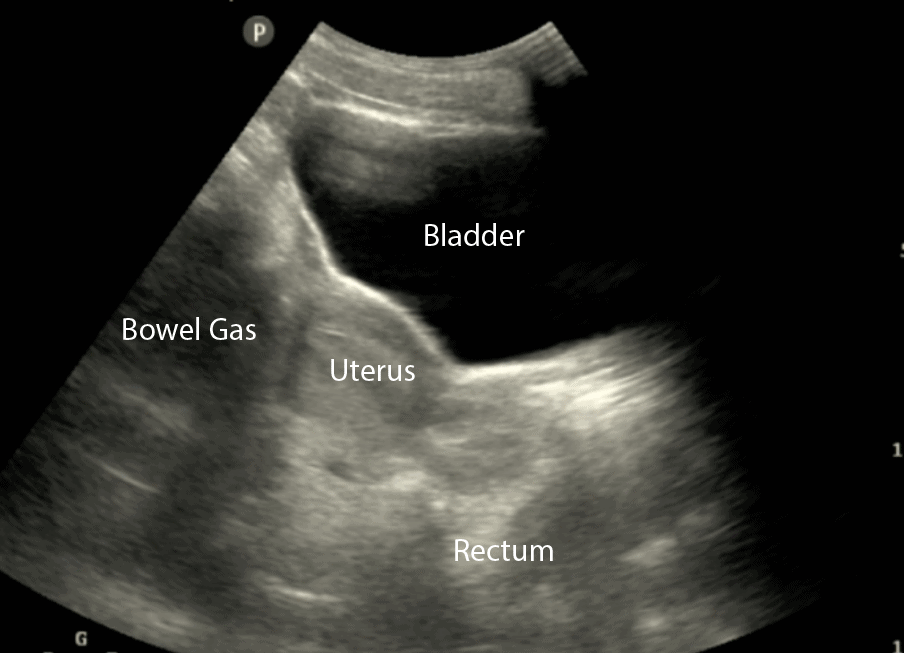
- In the longitudinal (sagittal) view, identify the Bladder, Bowel Gas, Uterus (females), Prostate (males), and Rectum.
- Observe the lateral borders of the bladder by tilting/fanning the probe left and right.
Step 2: Bladder Ultrasound – Transverse View
- Next, center the bladder and then rotate the transducer 90 degrees counterclockwise. The indicator should now point to the patient’s Right side.
- Make sure to tilt the ultrasound probe so it scans into the pelvic cavity.

- In the transverse view, identify the Bladder, Uterus (females), Prostate (males), and Rectum.
- Tilt/Fan the probe to examine the entire bladder from superior to inferior.
Step 3: Calculate Bladder Volume
POCUS 101 Tip: Ultrasound can be used to estimate bladder volume using a simple to remember formula: Height x Width x Length x 0.7
- The Width and Depth of the bladder are measured in the transverse view.
- The superior-inferior dimension (Height) is measured in the longitudinal view.
- Most ultrasound machines will automatically calculate the entire bladder volume which should be less than 300-400 mL in healthy adults and Post Void Residual (PVR) should be less than 50-100mL (Fitzgerald; Latini).
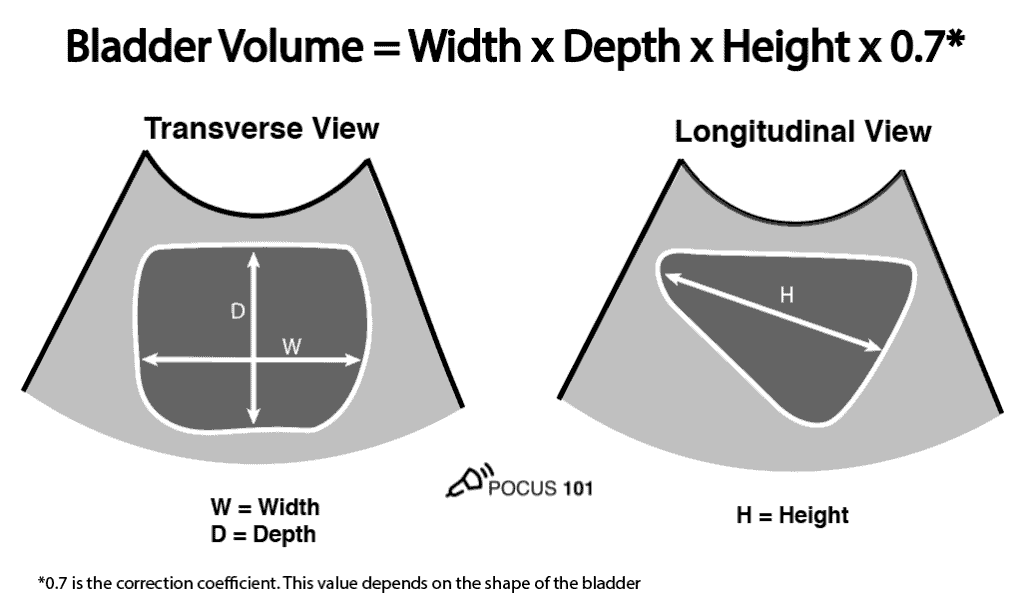
The actual formula used to calculate bladder volume is Width x Depth x Height x Correction Coefficient. If you want more accurate bladder volume measurements, you can use the correction coefficient that most closely corresponds to the patient’s bladder shape.
The table below shows you the correction coefficient for each of the bladder shapes:
| Bladder Shape | Correction Coefficient |
| Unknown | 0.72 (most commonly used) |
| Triangular prism | 0.66 |
| Cylinder (Ellipsoid) | 0.81 |
| Cuboid | 0.89 |
| Spherical | 0.52 |
Don’t want to remember all of these numbers? We created a Bladder Volume Calculator for you that will calculate the bladder volume for all of the different bladder shapes. For future reference, you can always access it here.
Bladder Volume Calculator
Bladder Pathology
Urinary Retention and Bladder Distension
Urinary retention occurs when a patient cannot completely empty their bladder. Common causes of bladder distention and/or retention include an enlarged prostate, bladder outlet obstruction, neurologic disorders, foley malfunction, or various medications.
Normal post-void residual (PVR) urine volume is <50 mL in patients, but <100 mL can be considered normal in patients older than 65 (Kelly 2004). The post-void residual volume is calculated using the ultrasound bladder volume formula described above or via urethral catheterization.
Performing a bladder ultrasound is recommended before catheterization because it is much more comfortable for the patient, less invasive, and avoids the risk of urethral trauma. Furthermore, performing an ultrasound for initial imaging to look for a distended bladder can help you evaluate if urethral catheterization will be necessary.
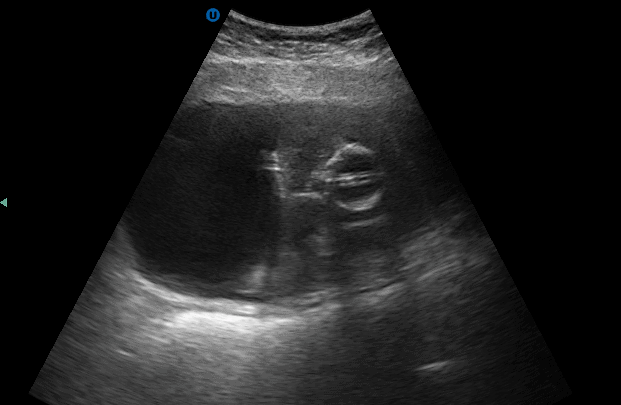
Catheter Foley Placement
A urinary foley catheter drains urine from the patient’s bladder. Your patient may need a catheter if he or she has urinary incontinence, prostate problems, or is preparing for surgery. At the end of the foley catheter lies a small balloon filled cuff with water that stabilizes the catheter inside the bladder.
Ultrasound is useful for checking that the foley catheter has been inserted properly and if it is draining urine properly.
Normal findings of a foley catheter on ultrasound will show an empty bladder with an inflated cuff.
If a foley catheter is malfunctioning or clamped, you will see the foley catheter in the bladder but with a distended bladder.
Bladder Ureteral Jets for Kidney Stones
Ureteral jets are a normal and periodic efflux of urine from the ureter into the bladder. Visualization of bilateral ureteral jets rules out complete obstruction of a specific ureter with high specificity (Strehlau).
- To see ureteral jets, scan slowly through the bladder in the transverse view and focus on the trigone (located on the posterior wall of the bladder).
- Turn on color Doppler or power Doppler while scanning the bladder in the transverse view. It may take 5-10 minutes before you can visualize bilateral jets so be patient.
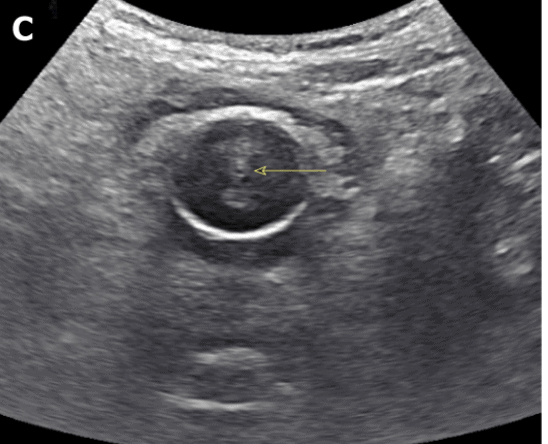
Bladder Stones
Bladder stones are often seen after renal stones travel from the ureters into the bladder. Bladder stones can also form in the bladder itself due to bladder stasis in patients with chronic urinary retention (Tublin, 2001).
On ultrasound, these stones appear hyperechoic and mobile with acoustic shadowing. If the stone is stuck in the ureterovesical junction (the junction between the ureter and the bladder body), the patient may also present with unilateral hydronephrosis.
Bladder Masses
Bladder masses are generally echogenic, irregularly shaped, and are found either mounted on the bladder wall or in areas of irregularly increased bladder wall thickness.
The majority of bladder masses are from transitional cell carcinoma. However, other causes include bladder diverticulitis, congenital outpouching of the bladder wall, and bladder wall thickening. Any sign of a bladder mass requires further urologic evaluation, and possibly cystoscopy and further imaging.
Since blood clots can be mistaken for bladder masses, irrigation of the bladder followed by another ultrasound scan is recommended (Geertsma et al). Blood masses are often mobile so it is recommended to have the patient roll onto their sides during the follow-up scan. If a blood clot is present, it should move as the patient changes position.
References
- Chan H. Noninvasive bladder volume measurement. J Neurosci Nurs. 1993;25(5):309-312. doi:10.1097/01376517-1993 10000-00007
- Fitzgerald MP, Stablein U, Brubaker L. Urinary habits among asymptomatic women. Am J Obstet Gynecol. 2002;187:1384–8.
- Latini JM, Mueller E, Lux MM, et al. Voiding frequency in a sample of asymptomatic American men. J Urol. 2004;172:980–4.
- Geertsma, Taco. “Pitfalls.” Urinary Tract and Male Reproductive System | 2.2 Bladder : Case 2.2.1 Bladder Tumors | Ultrasound Cases, www.ultrasoundcases.info/pitfalls-5215/.
- Kelly, Christopher E. “Evaluation of Voiding Dysfunction and Measurement of Bladder Volume.” Reviews in Urology, MedReviews, LLC, 2004, www.ncbi.nlm.nih.gov/pmc/articles/PMC1472847/.
- Koratala, Abhilash. “Point of Care Renal Ultrasonography for the Busy …” Www.wjgnet.com, Baishideng Publishing Group Inc., 28 June 2019, www.wjgnet.com/2220-6124/full/v8/i3/44.htm.
- “Obstructed Foley.” Obstructed Foley | Emory School of Medicine, med.emory.edu/departments/emergency-medicine/sections/ultrasound/image-of-the-fortnight/abdominal/obstructed_foley.html.
- Shenot, Patrick J., et al. “Urinary Retention – Genitourinary Disorders.” Merck Manuals Professional Edition, Merck Manuals, www.merckmanuals.com/professional/genitourinary-disorders/voiding-disorders/urinary-retention.
- Strehlau J, Winkler P, de la Roche J. The uretero-vesical jet as a functional diagnostic tool in childhood hydronephrosis. Pediatr Nephrol. 1997;11(4):460-467. doi:10.1007/s004670050317
- Tublin, M, and W Thurston. “The Kidney and Urinary Tract.” Diagnostic Ultrasound, 4th ed., Elsevier, 2001.
- Bih, L., Ho, C., Tsai, S., Lai, Y., Chow, W. (1998). Bladder shape impact on the accuracy of ultrasonic estimation of bladder volume Archives of Physical Medicine and Rehabilitation 79(12), 1553-1556. https://dx.doi.org/10.1016/s0003-9993(98)90419-1
- Bladder Stone: Case courtesy of Dr Maulik S Patel, Radiopaedia.org. From the case rID: 32815