Proper fluid management while avoiding fluid overload can be one of the most difficult parts of practicing medicine. Unfortunately, many physicians using Point of Care Ultrasound (POCUS) mainly rely on Inferior Vena Cava (IVC) measurements to predict the “Fluid Status” (either deficient or overloaded) of their patients.
If you are guilty of this, don’t worry, the majority of people are. It’s probably because you just didn’t have a better way to help assess the fluid status of your patients other than IVC measurements.
However, solely using IVC measurement has many problems. IVC measurements are inaccurate because, just like central venous pressure (CVP), they do not accurately represent your patient’s preload in the left ventricle. The IVC can also be dilated in conditions such as valvulopathies, pulmonary hypertension, or in patients with no comorbidities (such as athletes). Therefore a dilated IVC does not necessarily mean your patient is “fluid overloaded.” In addition, IVC dilation does not quantify the amount of venous congestion from other vital organs such as the lungs, liver, gut, and kidneys.
Most of us can agree that the development of venous congestion in the lungs (pulmonary edema) from fluid overload can lead to poor patient outcomes. This can be fairly easily seen using lung ultrasound or chest radiography. However, few us actually know how to evaluate other organs that can be affected by venous congestion such as the liver, gut, and kidneys. This is important because understanding early signs of venous congestion can help you limit fluid administration, look for underlying causes of right heart failure, start appropriate vasopressor therapy, and decrease the risk of significant end-organ damage such as acute kidney injury.
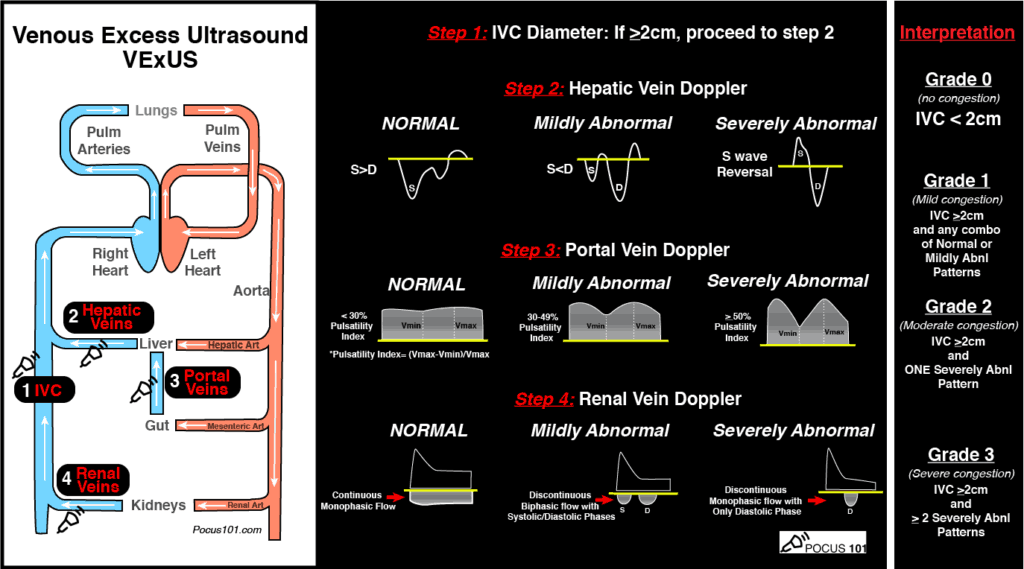
To help us with this, doctors William Beaubien-Souligny, Philippe Rola, Korbin Haycock, Rory Spiegel, et al developed a 4-step ultrasound protocol: the Venous Excess Ultrasound (VExUS) Score is an exam that evaluates and scores the severity of venous congestion of not just the IVC but also the liver, gut, and kidneys. You can download their VExUS book chapter at the end of this post if you wish.
Furthermore, they were able to validate the VExUS Score in a recent study and showed a correlated increased risk of AKI with an increased grade of venous congestion syndrome (SPOILER: if you read the article, the VExUS C profile performed the best and what is described in this post).
However, after going through the book chapter and the research study for our trainees (ICU fellows and residents), I found that it can seem daunting or confusing for some people to try to go through all of the material. Therefore, I wanted to write up this blog post with a Downloadable PDF VExUS Score Pocket Card and a detailed step by step approach to help make learning how to perform the VExUS Ultrasound protocol more feasible for you!
After reading this post you will:
- Have Access to Free PDF VExUS Ultrasound Score Pocket Card
- Have Access to a VExUS Ultrasound Score calculator to automatically calculate venous congestion grade
- Know exactly how to do the 4-steps of the VExUS protocol (IVC, Hepatic Vein, Portal Vein, and Intrarenal Vein Dopplers)
- Apply the VExUS ultrasound grading system criteria to your patients to help with fluid management
I want to especially thank Dr. Korbin Haycock for reviewing this material for accuracy, please follow him on Twitter! Also a shoutout to @NephroPocus on introducing me to a great VExUS diagram that I adapted into the PDF VExUS pocket Guide.
Alright, let’s get the VExUS Exam down!
Table of Contents
VExUS Ultrasound Score Pocket Guide PDF
Download VExUS Ultrasound Score PDF HERE
VExUS Ultrasound Score Calculator
You can always access the VExUS Ultrasound Score Calculator HERE as well for future reference.
When to use POCUS for Venous Congestion
Evaluation for venous congestion using Point of Care Ultrasound (VExUS POCUS) can be performed when trying to assess the fluid status of the patient. This can be especially important in our septic shock, congestive heart failure, and acute renal failure patients to help give us more data points towards starting fluids, stoping fluids, diureses, or vasopressor choice.
This exam should be done in conjunction with the clinical picture, lab values, and hemodynamic status of the patient. It should also be combined and interpreted along with cardiac ultrasound findings when possible.
The VExUS Score can give you evidence of venous congestion in the liver, gut, and kidneys to help predict early signs of end-organ damage and allow you to change/optimize your fluid management approach for your patient. It can also prompt you to look for the etiologies of your venous congestion such as causes of right heart failure.
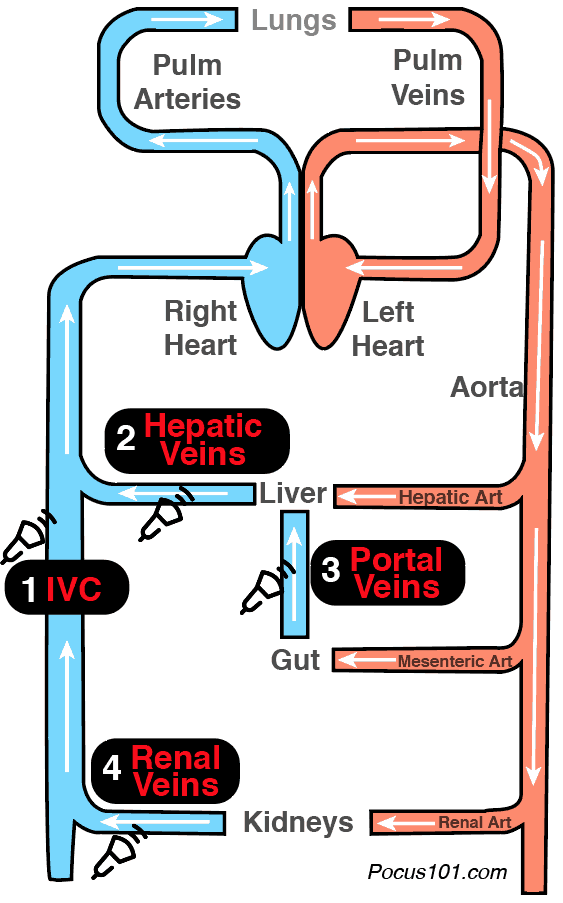
Organs to Evaluate Using the VExUS Ultrasound Score Protocol
Below are the organs you will be evaluating using the VExUS Ultrasound Protocol (aka Protocolo Vexus). As you can see, you can get a glimpse of venous congestion from several points prior to blood entering the right heart.
- Inferior Vena Cava
- Liver (hepatic veins)
- Gut (portal veins)
- Kidneys (intrarenal veins)
Machine Preparation
- Ideally, place the machine on the patient’s right side so you can scan with your right hand and manipulate ultrasound buttons with your left hand.
- Transducer: Ideally use a curvilinear probe since it can give better resolution of the vessels, but a phased array probe can be used as well
- Preset: Abdominal
- The Indicator should be on the left side of the screen
- You must have Pulse Wave Doppler capability on your ultrasound system. Most cart-based systems have this. Unfortunately, most hand-held ultrasounds don’t have Pulse Wave Doppler.
Patient Preparation
- Head of the bed should be down
- The patient should be supine
- Have patient bend legs relax the abdominal area to facilitate scanning
VExUS Score Step 1: IVC Assessment
Acquiring the IVC view with Ultrasound:
Place the probe in the subxiphoid position and get the IVC in the long-axis view. Most people will know how to perform an IVC exam, but for a more in-depth tutorial on how to obtain the IVC view you can click HERE.
Interpretation of IVC Measurements:
Evaluate the size and collapsibility of the IVC.
If the maximum IVC diameter is <2cm, then there is no significant venous congestion (at least cardiac related). You can stop the exam here and the VExUS score is 0.
If IVC is >2cm then proceed to the next steps.
VExUS Score Step 2: HEPATIC Vein Doppler Assessment
Acquiring the Hepatic Vein View with Ultrasound:
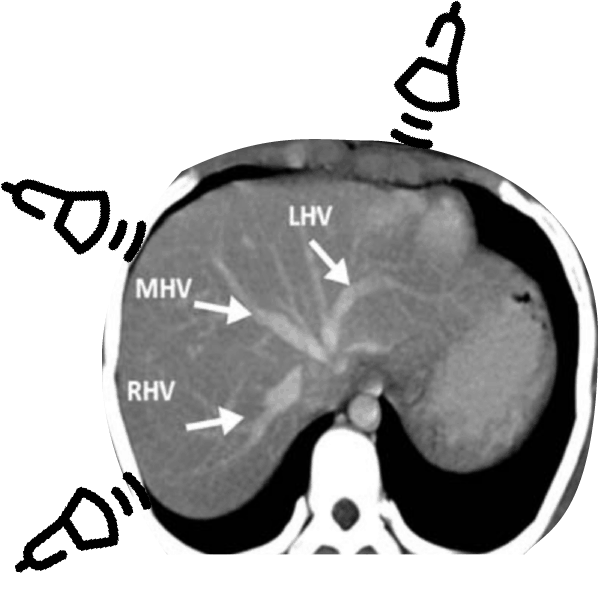
There are three hepatic veins: the right, middle, and left hepatic veins. You can use any of these veins to evaluate for hepatic vein Doppler patterns but the middle and right hepatic are usually the most accessible since the L hepatic vein view can be obscured by bowel/stomach gas. Below is a CT figure showing approximately where you should place your probe to target specific hepatic veins. Notice that it is NOT directly midline of the patient (I made this mistake when first trying to see the hepatic veins).
So here are the step to get the Hepatic Vein Doppler Tracings:
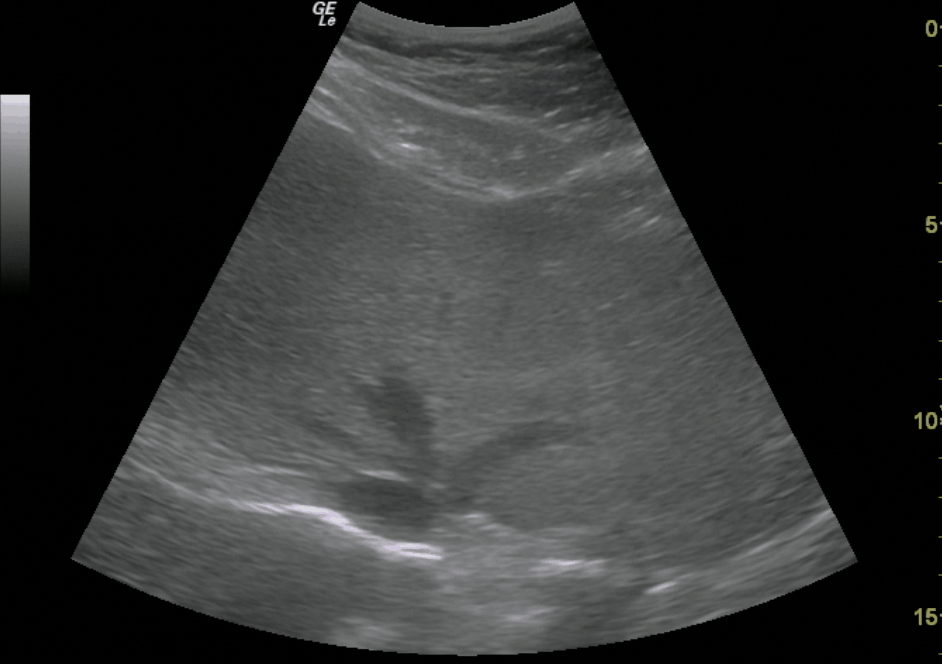
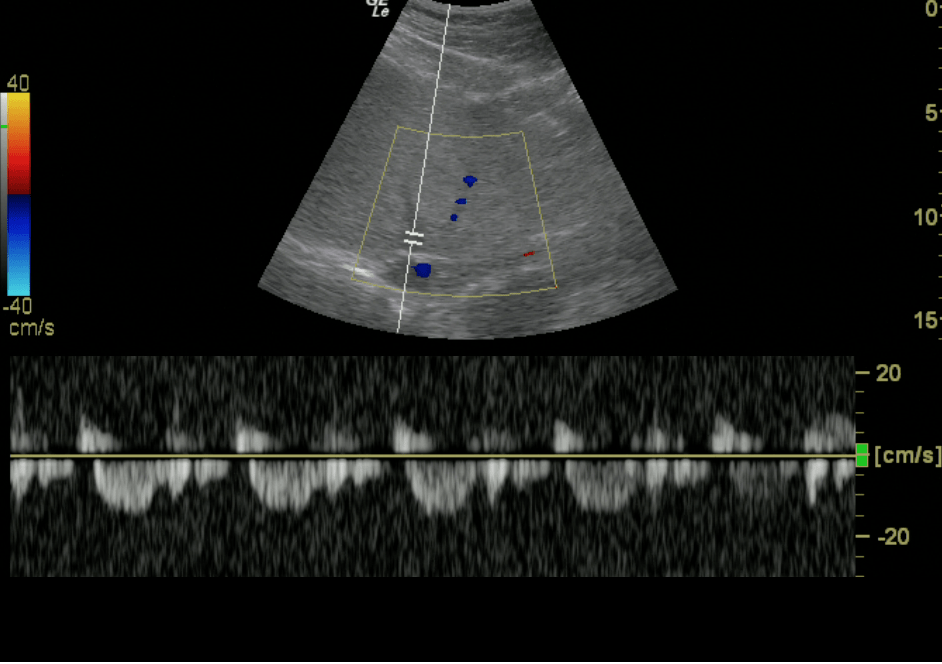
- Get a 2-D image of the IVC and hepatic veins.
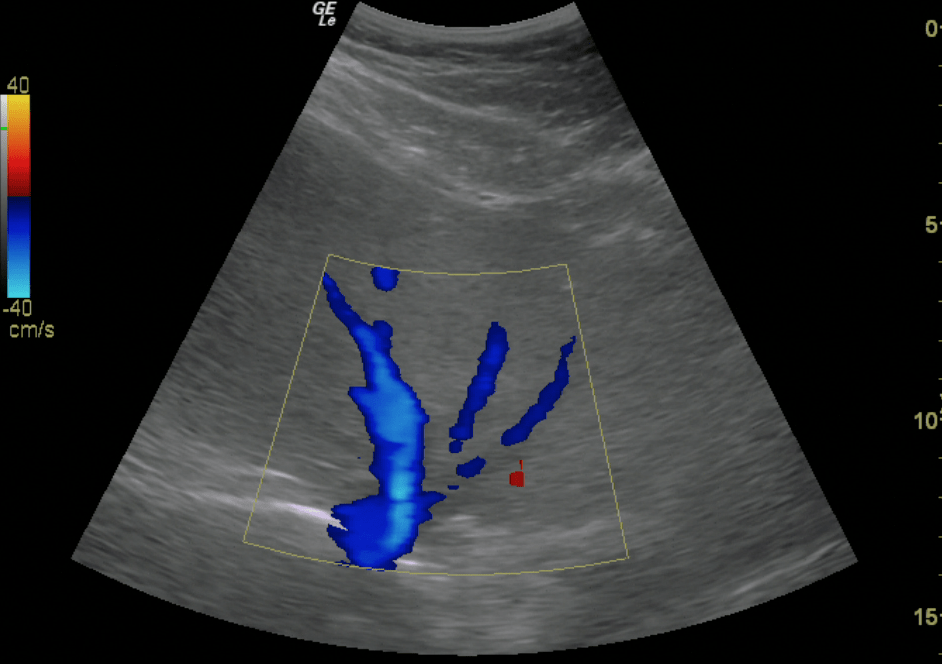
- Place color flow Doppler over the hepatic veins as they enter the IVC. You should see BLUE flow (away from probe)
- Place your pulse wave Doppler gate on a hepatic vein prior to it entering the IVC
- Initiate Pulse wave Doppler
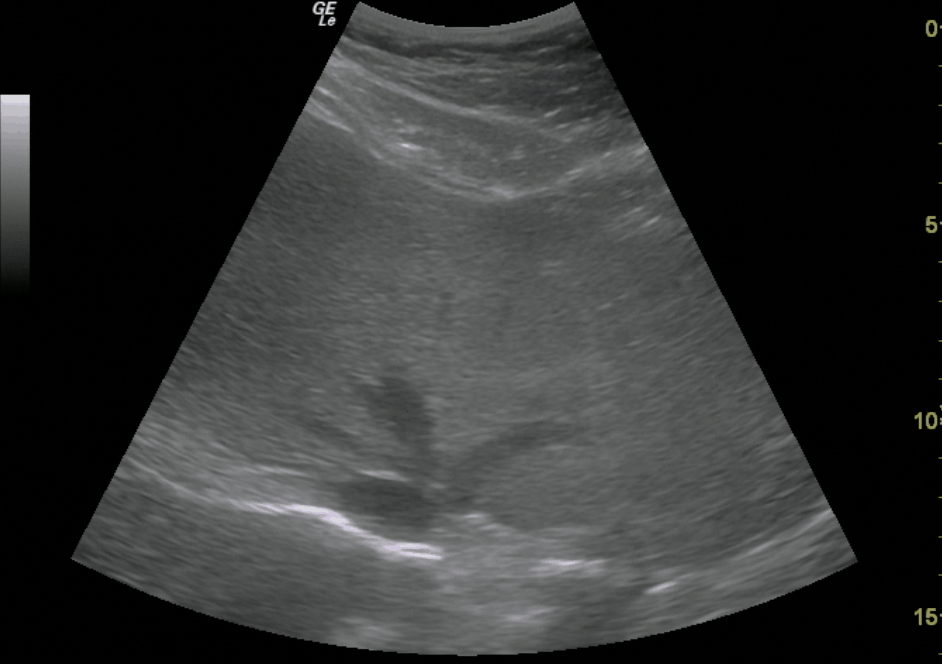
Hepatic Veins Entering IVC 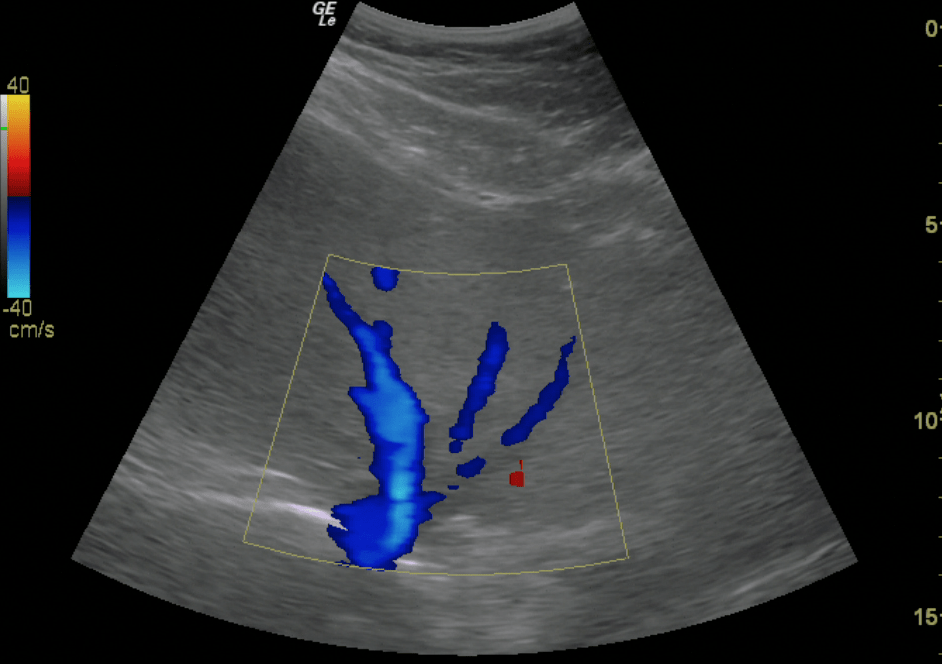
Hepatic Vein – Color Doppler 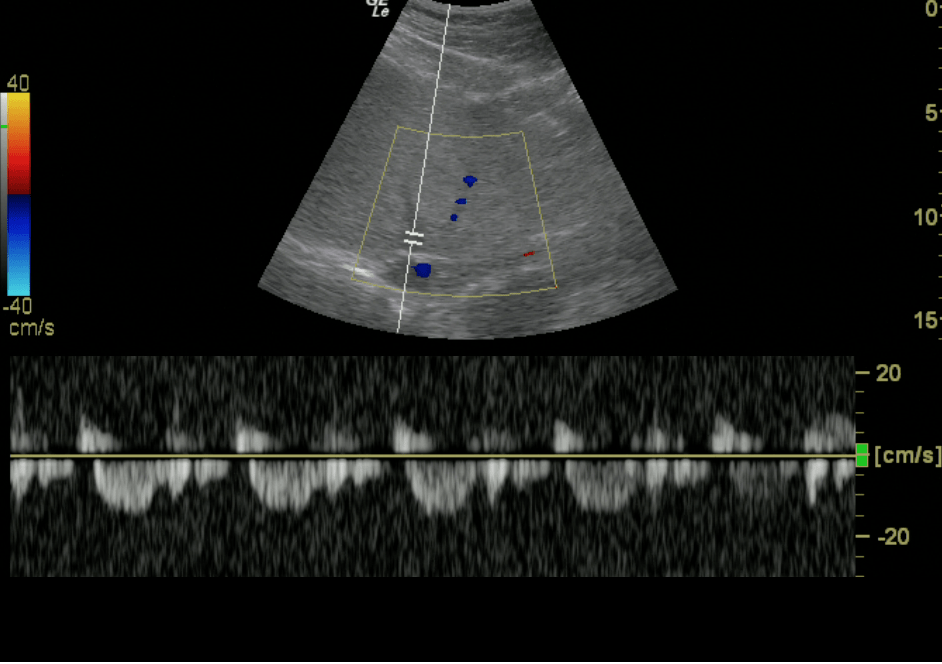
Hepatic Vein – Normal Doppler Pattern
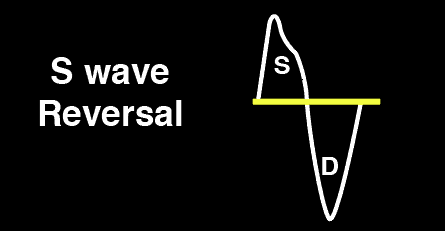
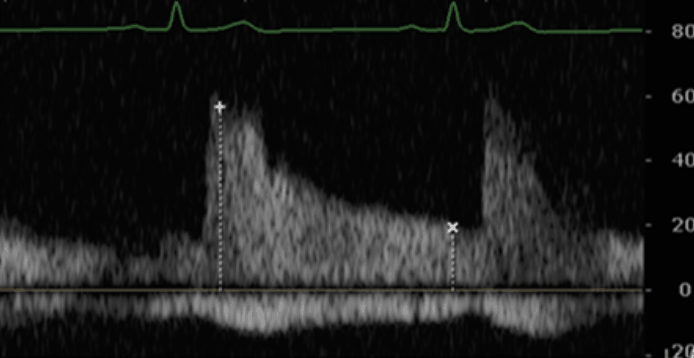
Interpretation of Hepatic Vein Doppler findings:
The hepatic vein Doppler is composed of a systolic (S wave) and diastolic (D wave). As venous congestion increases, there will be alterations of these waves with these typical patterns:
Normal Hepatic Vein Doppler: S>D
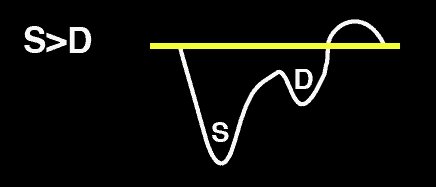
Mild Hepatic Vein Abnormality: S<D
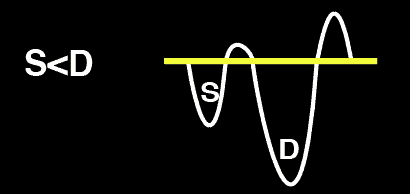
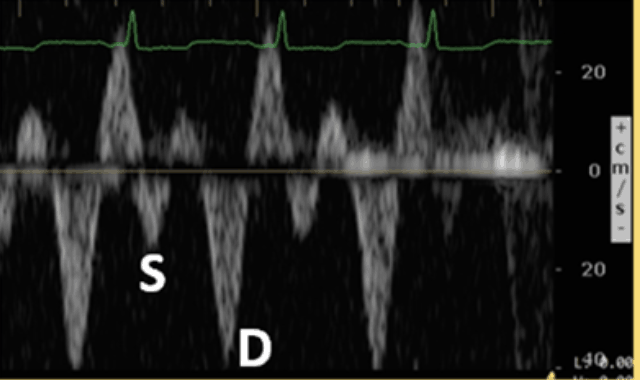
Severe Hepatic Vein Abnormality: S Reversal
VExUS Score Step 3: PORTAL Vein Doppler Assessment
Acquiring the Portal Vein View with Ultrasound:
I find that the portal vein is probably the easiest vein to find (compared to the hepatic and intrarenal veins). This can be done by placing your probe in the right midaxillary line.
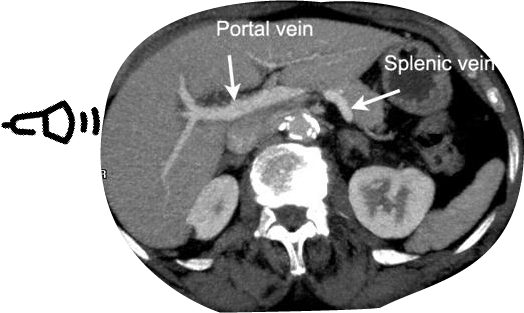
So here are the step to get the Hepatic Vein Doppler Tracings:
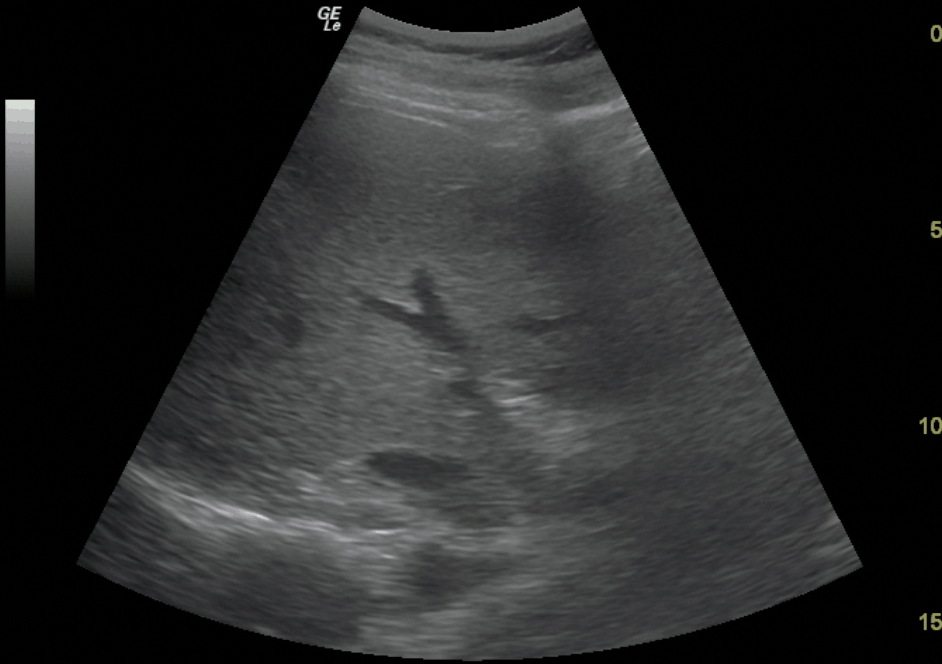
- Get a 2-D image of the Right Portal Vein
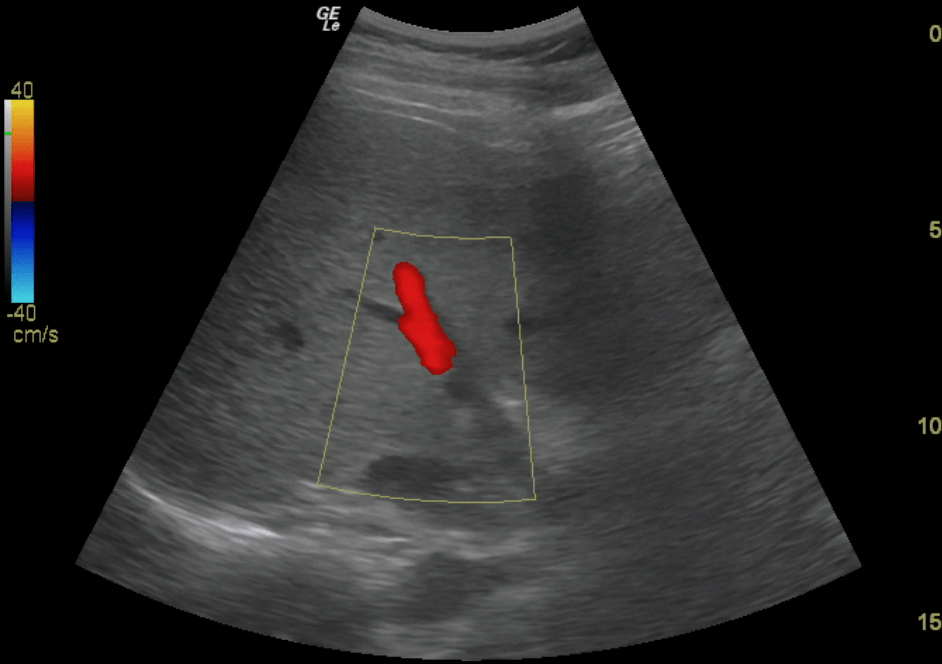
- Place color flow Doppler over the Right Portal Vein. You should see RED flow (towards the probe)
- Place your pulse wave Doppler gate on the Right Portal Vein
- Initiate Pulse wave Doppler
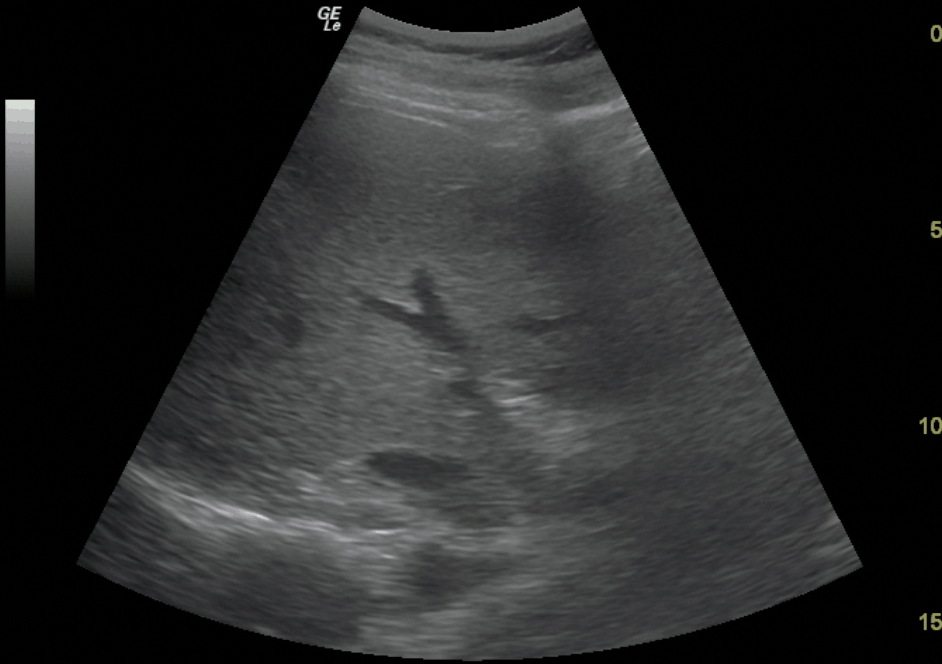
Portal Vein 2-D 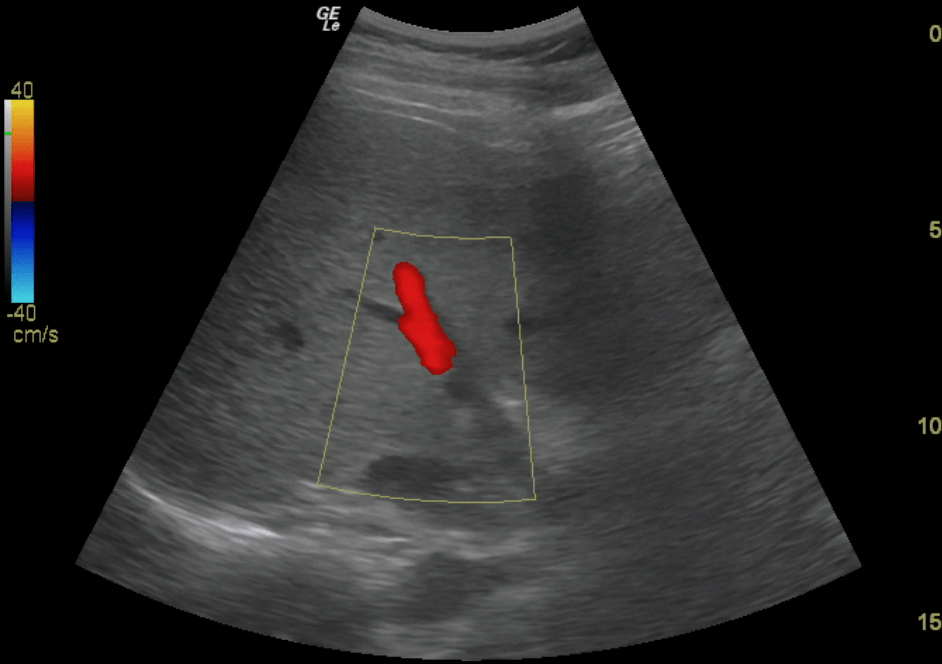
Portal Vein – Color Doppler 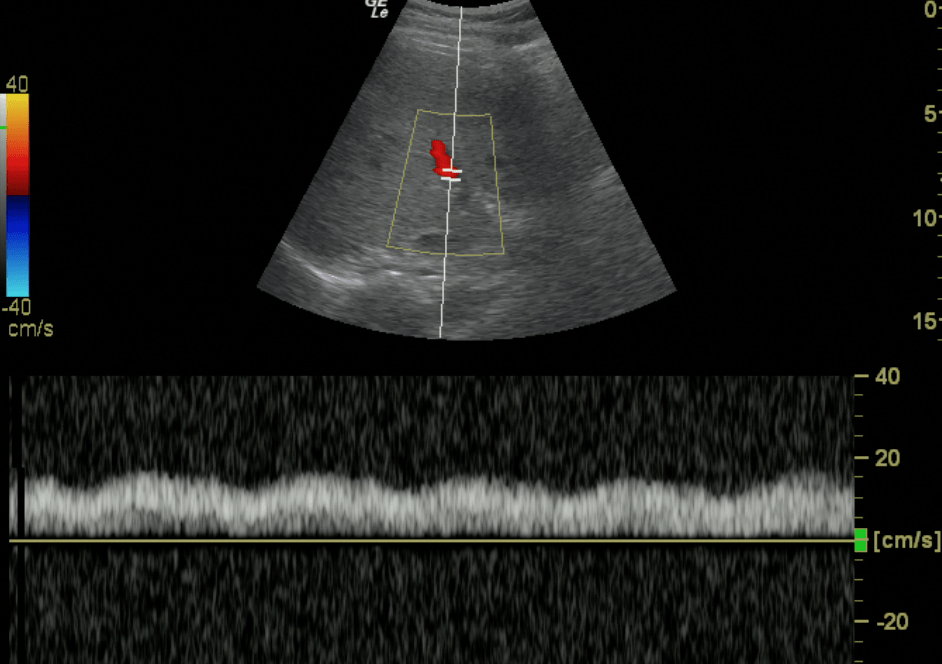
Portal Vein – Normal Doppler Pattern
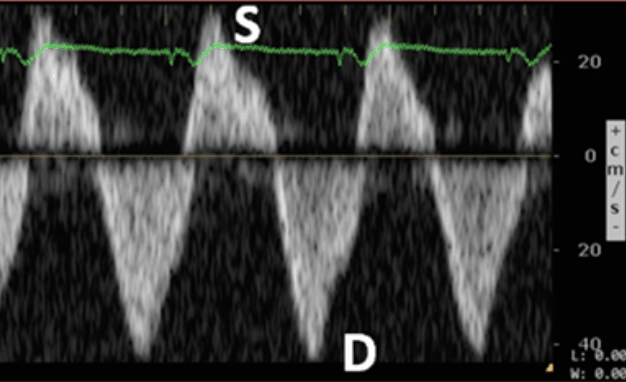
Interpretation of VExUS Score Ultrasound Portal Vein Doppler findings:
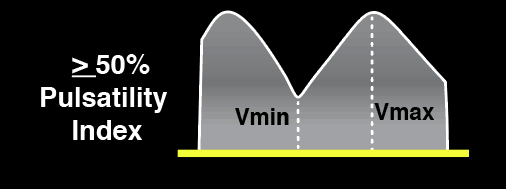
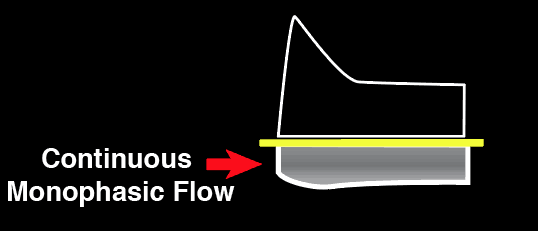
The Portal vein Doppler is normally monophasic with little to no variation. As venous congestion increases, there will be increasing amounts of pulsatility that is observed. The Pulsatility Index = (Vmax – Vmin)/Vmax.
Normal
Portal Vein Doppler
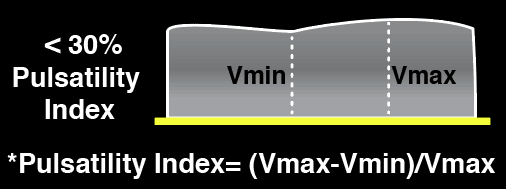
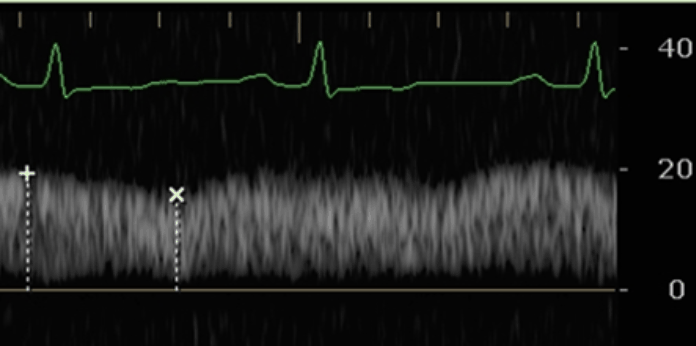
Mild Portal Vein Abnormality
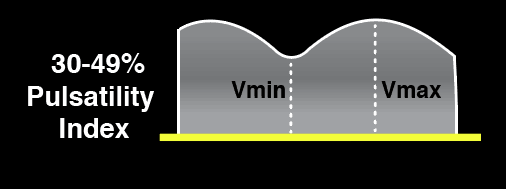
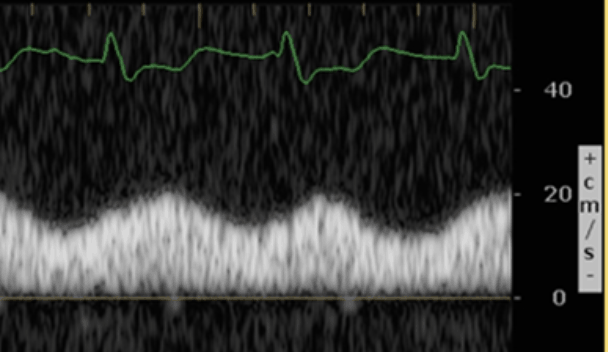
Severe Portal Vein Abnormality
VExUS Score Step 4: Intrarenal Venous Doppler Assessment
Acquiring the Intrarenal Vein View with Ultrasound:
The intrarenal vein assessment is probably the most difficult assessment to do out of all of the vessels. This is because the intrarenal veins are fairly small and the patient’s breathing patterns may limit your views. But don’t be discouraged and keep trying your best to get these views. With practice, you will get better at acquiring them.
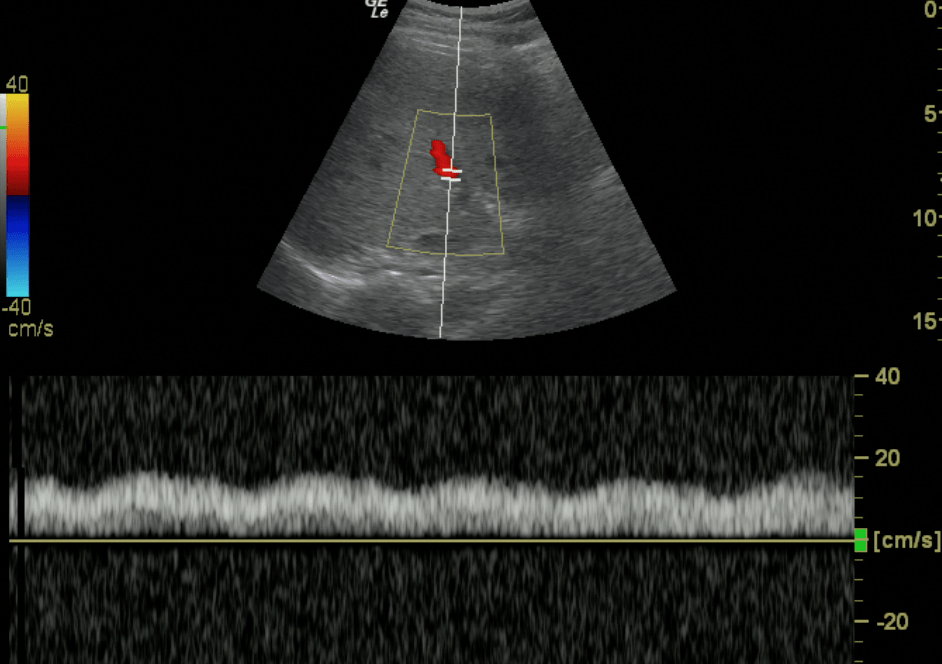
View the kidneys on either side at the posterior axillary line. Turn on the color Doppler and then look for the Interlobar vessels. Place the pulse wave Doppler gate where you see the best color Doppler signal and activate pulse wave Doppler. TIP: You may need to adjust the color and pulse wave Doppler scale and gain to get optimal settings. I have found having the Color Doppler scale around 10-25 cm/s is ideal.
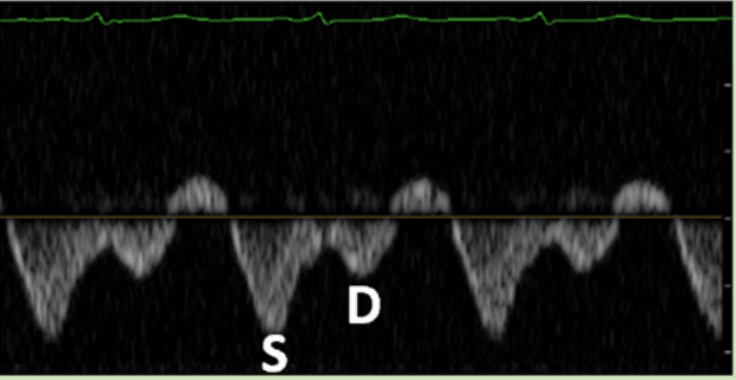
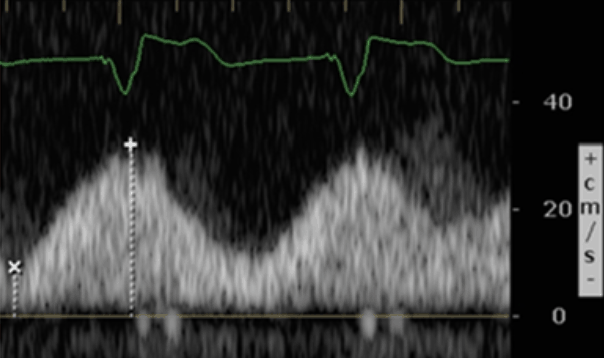
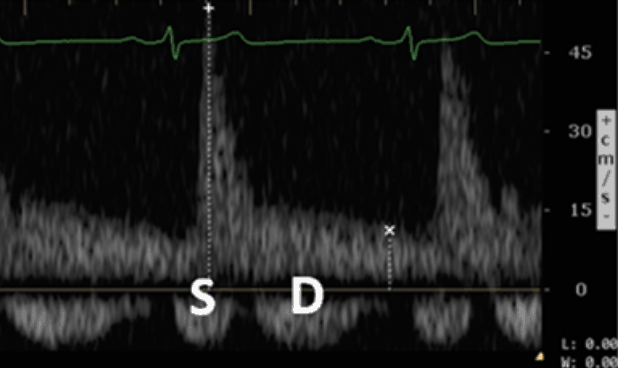
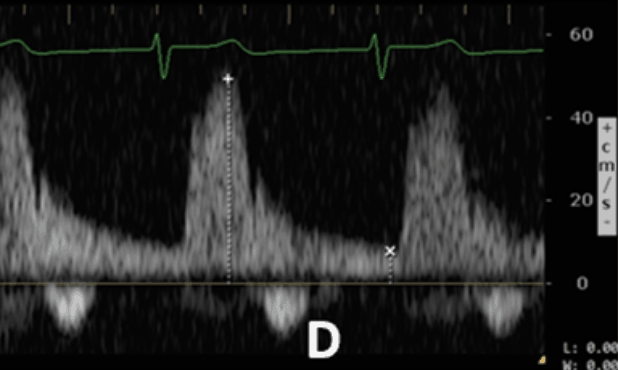
The vessels are so small that you will be able to detect BOTH the arterial and venous flow of the intrarenal vessels in the same view. For the VExUS exam, you will mainly be focusing on the venous component (the bottom portion of the Doppler tracing). Here is a brief video showing you how to do this:
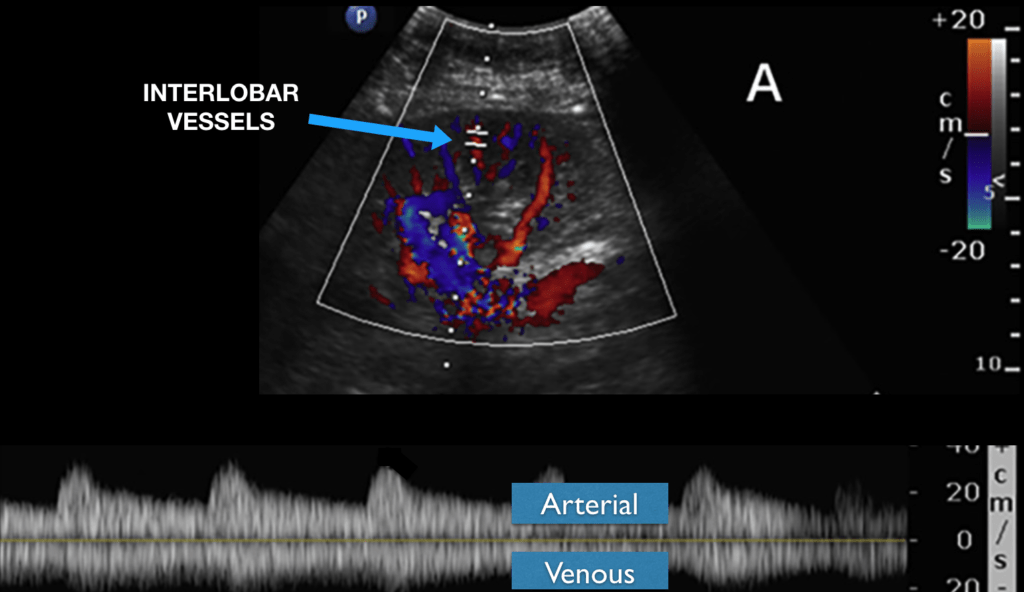
Interpretation of Intrarenal Vein Doppler findings:
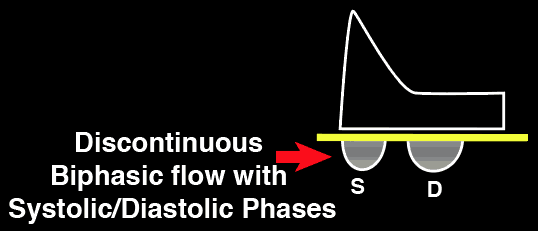
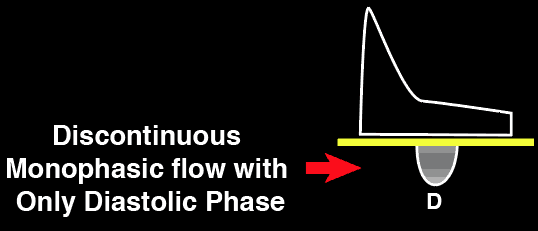
The Intrarenal vein Doppler pattern is usually a nice continuous monophasic flow. As venous congestion starts to increase there is a decrease in the systolic component of the wave with progression to biphasic (systolic/diastolic phases) and with renal congestion leading to complete absence of systolic flow showing only monophasic flow (only diastolic phase).
Normal Intrarenal Vein
Doppler
Mild Intrarenal Vein
Abnormality
Severe Intrarenal Vein
Abnormality
The VExUS Score – Putting Everything Together
This PDF puts everything together, including how to interpret the VExUS criteria and results. Also, remember you can access the VExUS Ultrasound Score Calculator HERE at any time if you forget how to score it.
VExUS Ultrasound Score:
- Grade 0: IVC <2cm = NO Congestion
- Grade 1: IVC >2cm with any combo of Normal or Mildly Abnormal Patterns = MILD Congestion
- Grade 2: IVC >2cm and ONE severely Abnormal Pattern = MODERATE Congestion
- Grade 3: IVC >2cm and >2 Severely Abnormal Patterns = SEVERE Congestion
Obviously, the VExUS Score is just another data point for your resuscitation endpoints you can obtain with Point of Care Ultrasound (POCUS). It doesn’t tell you exactly WHAT is causing the venous congestion but it can give you details of the relative severity of end-organ venous congestion syndrome your patient has. It then allows you to think about any potential underlying causes of venous congestion such as fluid overload, right heart failure, pulmonary hypertension, left ventricular dysfunction, etc. From there, you can use POCUS or other diagnostic modalities to help you elucidate and manage the underlying problems causing the venous congestion (VExUS syndrome) further.
I hope that was helpful and please leave any questions or comments below!
Download VExUS Ultrasound Score PDF HERE
References
- Marik, P., Baram, M., Vahid, B. (2008). Does central venous pressure predict fluid responsiveness? A systematic review of the literature and the tale of seven mares. CHEST 134(1), 172 – 178. https://dx.doi.org/10.1378/chest.07-2331
- Beaubien-Souligny, W., Rola, P., Haycock, K., Bouchard, J., Lamarche, Y., Spiegel, R., Denault, A. (2020). Quantifying systemic congestion with Point-Of-Care ultrasound: development of the venous excess ultrasound grading system The Ultrasound Journal 12(1), 16. https://dx.doi.org/10.1186/s13089-020-00163-w
- Goldhammer, E., Mesnick, N., Abinader, E., Sagiv, M. (1999). Dilated Inferior Vena Cava: A Common Echocardiographic Finding in Highly Trained Elite Athletes Journal of the American Society of Echocardiography 12(11), 988-993. https://dx.doi.org/10.1016/s0894-7317(99)70153-7
- Book chapter: Haycock, K., Spiegel, R. (2019). Special Skills: Venous Congestion.




Amazing post, am really happy to see how VExUS is spreading! I just have a couple comments that, for POCUS users which, I think and hope, are live physiologists at heart, it is important to understand that IVC measurement is highly accurate. The IVC doesn’t lie.(https://thinkingcriticalcare.com/2019/03/13/my-friend-the-ivc-foamed-foamer-foamus-foamcc/) It only misleads physicians who have wishful thinking that a single measure of any sort (CVP, weight, IVC, wedge, bla bla bla) would give you somehow simultaneously a measure of “volume status,” which none can. Each is a piece of hemodynamic data to be integrated in the clinical picture and requires a good clinician… Read more »
Thanks soo much Philippe! really appreciate the comment and appreciate all of the amazing work you are doing for the POCUS community!
Totally agree IVC doesn’t lie.
I believe most people are measuring IVC but just not interpreting it correctly, thinking dilated IVC always equal fluid overload instead of looking for valulopathies, RH failure, Pulm HTN, etc.
It’s also sad that some camps completely disregard IVC after the 7 mares article as well.
Thanks again Philippe!
Excellent work sir ,Good information
Excellent work
Thank you Dr. Sharma
Very nice post! TY very much! What its the most common pattern in the PV doppler of a cirrhotic Liver?
Hi Vicente! What a great question. There can definitely be different patterns of HV and PV depending on the severity and stages of Cirrhosis. Here is an EXCELLENT free open access article detailing all the different scenarios: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4701371/. Hope that helps!
Very nice article. i am pediatric intensivist . I am interested in VEXUS assessment and doing it in ventilated pediatric pt . i want to ask you regarding Vexus in pediatrics as there are many issues How to do it in tachycardic patients , in spontaneously breathing pt as they can not hold their breath , IVC measurement – is it ok to take distensibilty and coolapsibilty indices instead of diameter. Many a times in tachycardic pt hepatic vein doppler waveform – it difficult to asses which is S wave and which is D wave . can u please elaborate… Read more »
Hi Dr Ajay Walimbe! Thanks for the comment. I apologize I do adult critical care and emergency medicine. I don’t see kids normally so can not attest to pediatric physiology. The waveforms should be similar in pediatrics as far as I understand (assuming they are not neonates or have any shunt physiology). I would think that the findings of the VExUS study would be generalizable once a child is above 10 or 12 years of age. Yes tachycardic patients can present an issue (especially in kids) with identifying the S versus D wave. In these cases you should put an… Read more »
thanks a lot sir
Many thanks for this excellent contribution. Very innovative approach. I have a question of understanding. In step 2 (HEPATIC Vein Doppler Assessment) the left image shows the normal findings: Normal Hepatic Vein Doppler: S>D In the picture below, this pattern is shown as a B-scan. The B-scan also shows the ECG with the QRS complexes. If you draw a line down from the QRS, you see that the S-wave does not represent the systole, but the D-wave. If I understand the ECG correctly, it is an abnormality: S<D because the S wave is actually the D wave and the D… Read more »
Hi Thank you so much for this wonderful comment and insight on the VExUS Ultrasound Score Protocol! I totally agree with you on this. I’ve contacted the study authors to clarify this since those images are from the VExUS paper. I got a response back from them and they said the wave forms are indeed correct (S and D labeled correctly). They believe that there is an error in the EKG or there maybe a lag in the EKG reading compared to the Doppler signals. It is a normal waveform. Hope that clarifies your question. I will likely have to… Read more »
Yes, this is indeed a lag in the ECG trace. The US machine was connected to the monitor in the ICU when this trace was taken, rather than directly to the ECG leads, which caused the ECG and waveform to be out of sync. Nice catch Henryk!
Thanks Korbin for clarifying this EKG reading on the VExUS Score!
Hello, nice topic! As far as I understood, VExUS helps to quantify the amount of venous congestion from vital organs such as the liver, gut, and kidneys. It’s a prognostic score. Therefore, similr to IVC alone, an high VExUS score does not necessarily mean your patient is “fluid overloaded”. All must be integrated with echocardiography to define the etiologies. Can you confirm?
Hi Giacomo! Thanks for the comment. Yes it tells you the degree of venous congestion present and is an additional datapoint for resuscitation. I would say that if your patient has significant venous congestion, you will have to weigh the benefits fluid administration versus the severe harm of causing worsening venous congestion. From my experience, if you have significant venous congestion, additional fluid administration, finding the CAUSE of the venous congestion is important. For examples Pulm Embolism, Pulm Art HTN, Left sided heart failure, diastolic dysfunction etc. Therapy targeted towards the cause of venous congestion is helpful and can… Read more »
hi. its dr ajay pediatric intensivist. is this vexus score same for spontANEOUSLKY BREATHING PT AND Mechanically ventilated pt .
The VExUS study was validated in spontaneously breathing patients. However I have been implementing it with mechanically ventilated patients and it seems the results do correlate with the amount of venous congestion.
can we differentaite development of tension pneumothorax form nontension pneumothoarx by vexus. e.g pneumothorax diagnosed but vexus showing mild abnormalaity and progressing to more severe abnormality .
I would say that as tension PTX gets worse, there will be elevation of RVSP and RAP with resulting IVC enlargement/non-collapsibility. This should correlate with worsening VExUS score. However, personally I would just place a chest tube early on if I was concerned about possible progression. Most of the tension PTX I’ve seen progress very rapidly.
Nice topic!! Im a pediatric intensivist. How could the ivc measurement be modified in order to use this score in pediatric patients? Thanks you
Hi Diego! Great question. I mainly work with adults and the VExUS Ultrasound study was not validated on pediatric patients. Personally I would use any current literature for IVC cutoff in pediatric patients that is out there. This is a great article that may help: https://onlinelibrary.wiley.com/doi/10.7863/ultra.34.6.1091 From there you can look to see if they have abnormal wave forms! Hope that helps
Sincerely,
Vi Dinh (POCUS 101 Editor)
Very informative post. if Vexus score is increasing that means there is intravascular fluid overload and we should come down on fluids , remove fluids , diuretics .
But in sepsis, MIS-c , dengue there is capillary leak and initially there is interstitial edema leading to hepatomegaly, AKI. if we do venous Doppler in this capillary leak with organ interstitial edema what happens to organ arterial and venous Doppler .
Can we diffretertaite intravascular vs extravascular fluid overload by using ART and venous doppler as treatment is entirely different.
Hi Ajay! Thanks for the comment. From my understanding and my use of VExUS over the past year and a half, even if there is capillary leak, the VExUS score helps determine intravascular fluid overload regardless of the underlying condition (CHF, too much IVF administration, RV failure, etc). You can use the renal resistive index and look at the arterial flow of the kidney to predict AKI. Extravascular fluid overload will need other monitoring parameters in my opinion.
Hope that helps!
-Vi
Hi Vi,
Nice post! Good job.
As a experienced POCUS user I found it to complicated. Just first impression.
I completely agree with your opinion about IVC dilatation. There was in the American Focused Cardiac Ultrasound: IVC has 2 patterns: 1. hypovolemic and 2. non-hypovolemic.
Check the paper of Dr Gabrielle Via about IVC – it’s really interesting. From the many causes of the IVC distention the fluid overload is on the end of the list.
Take care!
Thanks so much. Appreciate the comment. Yes IVC is much more complicated than people make it to be. Appreciate the reference to the paper.
Nice works , very informative .
Thanks so much Adi!!
[…] POCUS 101 – VEXUS Ultrasound Score […]
[…] POCUS 101 – VEXUS Ultrasound Score […]
[…] effusions and ascites). More recently, the Venous Excess Ultrasound Score (VExUS) has emerged as a popular tool to assess venous congestion. VExUS is a scoring system developed in 2019 to identify and grade systemic congestion severity […]
[…] I recommend going through the Renal Fellow Network post by Dr. Argaiz as well as this one on POCUS 101 by Dr. Vi […]
Can we diffretertaite intravascular vs extravascular fluid overload by using ART and venous Doppler as treatment is entirely different. As in dengue with capillary leak portal vein velocity goes down <16. Can the vein be compressed if there is tissue edema due to capillary leak — that is if AKI due to capillary leak — increase in Arterial RI with low renal velocities with continuous venous form ( reverse vexus )
What CPTs are typically reported for the VExUs Scoring?
Hi Lamar! It would likely be a limited abdomen. You can check this post out: CPT Codes
[…] 補足 VExUS 引用)https://www.pocus101.com/vexus-ultrasound-score-fluid-overload-and-venous-congestion-assessment/ […]
Great article! I love the pdf pocket card. Can the VEXUS score be applied to intubated patients considering the effects of positive pressure ventilation/PEEP on the right heart/veinous system?
Thanks Jean-Luc! I’ve been using it on intubated patients and it seems to work. Jut make sure to get the waveforms during end expiration.
[…] Excess Ultrasound | (VExUS) Score | the 4-step ultrasound protocol developed by Dr. William Beaubien-Souligny, Philippe […]
Great job!!! This score improve my diagnosis and therapy daily! Fluid therapy is not always guided by pathophysiological reasoning, so ultrasound approach (LVOT-VTI, IVC, Vexus, subpleural pattern) is a fundamental aid for the initial phases of the management of the critically ill patient and for subsequent monitoring in sub-intensive and intensive care units . I would like to ask you if these scores can lead to universally shared therapies, in order to have precise values (amount of liquids, dosage of amines and diuretics, etc.).
Hi Noah! Thank for the comment. I think these scores just give you more data points that can help guide your therapies rather than a specific therapy that works for any and all patients. All of the modalities will have inherent limitations so the more data points you have the better understanding of what is going on with the patient. It’s also always important to reevaluate your patient after therapies and see if the patient is responding appropriately. Thanks again for reading! -Vi
Hi Vi. I noticed that at the bottom of the calculator, it says that results “Will populate after input of all fields”, however it seems that a grade is produced after the IVC is assessed and one other field is “Severe”. Do you recommend to complete all 4 assessments before producing a grade?
Hi Shannon if one of the fields is severe it will automatically grade based on the Vexus score. Hope that helps!